- LOGIN
- MemberShip
- 2025-12-19 05:40:35
- Policy
- Jardiance generics listed late October…but not CKD
- by Jung, Heung-Jun Oct 30, 2025 06:09am
- As the substance patent for Jardiance expired on October 24, a total of 235 products—both single-agent and combination formulations—were simultaneously added to Korea’s reimbursement list. However, Chong Kun Dang chose a different approach, applying for sequential listing of its single-agent and combination products. The company first listed its single-agent Empamax Tab (10 mg, 25 mg) on the reimbursement list in line with the patent expiration date this month and plans to add 13 combination formulations in November. According to industry sources on the 29th, unlike other generic manufacturers, Chong Kun Dang owns a salt-modified single-agent formulation, which led to this stepwise, sequential reimbursement strategy. Chong Kun Dang’s Empamax Tab (10 mg, 25 mg) contains empagliflozin L-proline. It is a salt-modified version of the original compound, unlike other generics. By conjugating L-proline, an amino acid, the company successfully avoided patent infringement. After review by the Health Insurance Policy Deliberation Committee, the products have been reimbursed since October 24 at the same price as their planned sales price. Starting in November, 13 additional combination formulations—both dual and triple combinations—will be listed. A total of 11 products, that are combinations of empagliflozin and metformin-Empamax XR Tab (10/1000 mg, 12.5/1000 mg, 25/1000 mg), Empamax M Tab (12.5/500 mg, 12.5/850 mg, 12.5/1000 mg, 5/500 mg, 5/850 mg, 5/1000 mg), and Empamax S Tab (10/100 mg, 25/100 mg- will be granted reimbursement. In addition, two triple-combination formulations containing empagliflozin + sitagliptin + metformin—marketed as Emsiformin XR Tab—will also be added. A Chong Kun Dang official explained, “We modified the salt form to enhance safety. Unlike other generics, we first listed the single-agent product, and our combination products are being reimbursed subsequently based on the single-agent drug data.” Chong Kun Dang has received marketing approval for a total of 18 products, including both single-agent and combination versions, but has submitted reimbursement applications for only 15. Some triple-combination formulations and specific dosages were not included in the application. The company plans to prioritize products with higher prescription potential. The official added, “We are first launching the dosages expected to have higher prescription volume, and will apply for additional listings depending on market conditions.”
- Company
- Reimb for Perjeta as adjuvant therapy under CDDC review
- by Eo, Yun-Ho Oct 29, 2025 06:12am
- The expansion of reimbursement coverage for Perjeta’s use as adjuvant therapy in breast cancer is drawing attention. According to industry sources, Roche Korea’s HER2-positive breast cancer treatment Perjeta (pertuzumab) has been submitted for review by the Health Insurance Review and Assessment Service (HIRA) Cancer Disease Deliberation Committee. Currently, Perjeta is reimbursed for treating HER2-positive metastatic or unresectable locally recurrent breast cancer. In early breast cancer, it is granted selective reimbursement as a neoadjuvant therapy (before surgery), with patients bearing 30% of the cost. However, in the postoperative adjuvant therapy stage—a key treatment step to prevent recurrence—has remained non-reimbursed (100% patient coinsurance) since its indication was added in Korea in 2018, limiting patient access. The recent submission to the National Health Insurance Service's Drug Disease Deliberation Committee is believed to have been significantly influenced by the 10-year long-term follow-up data from the Phase III APHINITY clinical trial, presented at the European Society for Medical Oncology Breast Cancer Conference (ESMO Breast Cancer 2025) last May. This study newly confirmed statistically significant final overall survival (OS) data for the combination of Perjeta and Herceptin (trastuzumab). When Perjeta was administered in combination with Herceptin and chemotherapy, the risk of death in patients with HER2-positive early breast cancer was reduced by 17% compared to the existing Herceptin-chemotherapy combination therapy. Furthermore, the 10-year survival rate in the Perjeta-Herceptin treatment arm was 91.6%, showing an improvement compared to the 89.8% in the control arm. The Perjeta-Herceptin treatment arm also demonstrated greater clinical benefit in patients at high risk of recurrence. Specifically, in a subgroup analysis of patients with lymph node–positive disease, who are at high risk of recurrence, the combination showed a 21% reduction in the risk of death. Furthermore, the benefit in invasive disease-free survival (iDFS) was also maintained, reaffirming the earlier findings of the APHINITY study. It remains to be seen whether Perjeta's adjuvant therapy indication can pass CDDC review and ultimately be granted reimbursement coverage. Meanwhile, the Perjeta and Herceptin combination is currently recommended as Category 1 adjuvant therapy in the U.S. NCCN Guidelines for patients with HER2-positive early breast cancer and lymph node metastasis. It is also recommended as Category 1 adjuvant therapy for high-risk, lymph node–positive patients who achieved pathological complete response (pCR) after neoadjuvant chemotherapy.
- Company
- Will the Indian API cause problems?
- by Kim, Jin-Gu Oct 29, 2025 06:12am
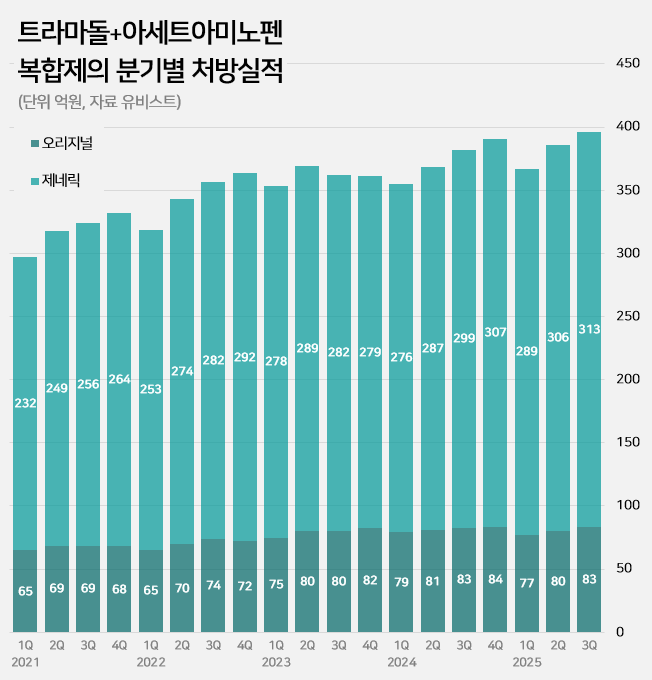
- An impurity issue has emerged as a major variable in the tramadol-acetaminophen combination drug market, valued at approximately KRW 150 billion annually. Following the detection of impurities in three generic products using Indian-sourced active pharmaceutical ingredients (API), the pharmaceutical industry is watching closely for the potential expansion of the impurity issue across all API from India. In this case, the market is expected to be reorganized around products that use non-Indian sourced API. 85% of tramadol DMFs are produced in India...Concerns Over Widespread Impurity Detection According to the Ministry of Food and Drug Safety (MFDS) on October 29, following the excess detection of the impurity NNDT (N-nitroso-desmethyl tramadol) in a tramadol monotherapy product in July, the recall target has recently been expanded to include tramadol + acetaminophen combination products. To date, impurities have been detected in three tramadol + acetaminophen combination products. The MFDS issued recall orders for specific batch number products of: ▲Dongkoo Bio & Pharma’s 'Jimuradol Tab' ▲Ausco Korea Pharma's 'Acetadol Tab' ▲Union Korea Pharm’s 'Atracen Tab.' All three products in which impurities were detected are known to have used India-sourced API. The concern is that a significant portion of the tramadol + acetaminophen combination products currently distributed in South Korea relies on API sourced from India. Currently registered sources of tramadol API: YELLO-India, BLUE-Israel, RED-Switzerland, GREEN-Korea Indeed, examining the Drug Master File DMF status for tramadol-related API shows that 62 of the 73 registered raw material manufacturers (85%) are located in India. The remaining 11 sites include 8 in Israel (11%), 2 in Switzerland (3%), and 1 in Korea (1%). Many domestically supplied products likely rely on Indian-sourced API. KRW 150 Billion Market...Top-selling products not at risk of impurity expected to benefit The three products where impurities were detected have negligible prescription sales. According to pharmaceutical market research firm UBIST, the cumulative prescription sales for these three products combined were less than KRW 400 million in the third quarter of this year. While the market impact is currently limited, analysis suggests that market restructuring will be unavoidable if impurity detection expands across Indian-sourced API. This is because securing new raw material manufacturers outside of India is difficult, and the administrative process for changing API registration alone takes approximately six months, which would lead to a market supply gap. The tramadol + acetaminophen combination market in Korea has seen steady growth in the moderate-to-severe pain treatment sector. It increased by 24% over the last four years, from KRW 120.7 billion in 2020 to KRW 127.1 billion in 2021, KRW 138.2 billion in 2022, KRW 144.6 billion in 2023, and KRW 149.6 billion last year. Cumulative sales reached KRW 114.9 billion in the third quarter of this year. Quarterly prescription sales of tramadol-acetaminophen combination drugs (DARK GREEN: original product, LIGHT GREEN: generic products; unit: KRW 100 million, source: UBIST). The original product, Janssen Korea's Ultracet, recorded cumulative sales of KRW 24.1 billion in the third quarter, a slight decrease from KRW 24.3 billion in the third quarter of last year. Generic products collectively saw a 5% increase in the same period, rising from KRW 86.3 billion to KRW 90.9 billion. The growth of top-selling generics was particularly notable: Samjin Pharm's 'Synerjet' grew by 23%, from KRW 6.9 billion to KRW 8.6 billion; Myung Moon's 'Traphen' grew from KRW 5.2 billion to KRW 6.6 billion; and Genuone Sciences' 'Painless' increased from KRW 4.4 billion to KRW 5.1 billion. In this circumstance, if the impurity issue spreads, non-detected products are expected to quickly replace the market. Currently, the market-leading products are understood to be not at risk. The original product, Ultracet, has registered a Swiss manufacturer as its API supplier. The top generic product, Samjin Pharm's Synerjet, manufactures its finished drug in-house using an Israeli-sourced API. Neither of these two products was requested to submit data in the MFDS's comprehensive investigation of NNDT impurities in tramadol.
- Policy
- Non-reimbursed approvals of off-label drugs
- by Jung, Heung-Jun Oct 29, 2025 06:10am
- The number of non-reimbursed approvals of off-label drugs: while 208 applications for off-label use were rejected, 2,186 were approved between 2020-2025.The number of approvals for non-reimbursed use of drugs beyond their authorized indications (off-label) has been more than 10 times the number of rejections over the past six years. While 208 applications for off-label use were rejected, 2,186 were approved, often because the benefits outweighed the risks. On October 27, the Health Insurance Review & Assessment Service (HIRA) publicly disclosed, for the first time, the number of non-reimbursed approvals for off-label drugs, including over-the-counter (OTC) medicines. Applications for non-reimbursed off-label drug use must first be reviewed by an IRB (Institutional Review Board) established in a hospital or by an academic society. For OTC medicines, HIRA commissions the Ministry of Food and Drug Safety (MFDS) to review safety and efficacy, while anti-cancer drugs are approved by the Cancer Disease Review Committee (CDRC), which holds monthly. Unlike anti-cancer drugs, only the records of rejections for OTC medicines had been disclosed until now. This had been criticized as a problem, making it difficult for healthcare institutions to file applications for off-label non-reimbursed use. There was also a persistent request to disclose approval records for OTC medicines to ensure fairness. HIRA pre-announced a partial amendment to the 'Partial Revision to Operational Regulations for Approval of Non-Reimbursed Off-Label Drug Use' in September and proceeded with public consultation. The newly disclosed approval cases totaled 2,186 from 2020 to the present, broken down as follows: 472 cases in 2020, 572 in 2021, 266 in 2022, 485 in 2023, 276 in 2024, and 115 this year. Meanwhile, a total of 377 rejection cases were disclosed over 13 years, from 2013 to 2025. Specifically, from 2020, when approval cases began to be disclosed, 208 cases were rejected. Examining the trend of rejections by year shows: 33 rejections in 2020, 86 in 2021, 38 in 2022, 44 in 2023, 6 in 2024, and 1 this year. This data indicates a significant reduction in rejection cases over the last two years. The disclosed rejection data for this year includes one additional rejection for Mabthera (rituximab). The application was filed citing expectations that the drug would be more cost-effective, have fewer side effects, and offer higher therapeutic efficacy than alternative drugs. Yet, it was denied because the submitted evidence did not substantiate the claims.
- Policy
- MOHW ‘will support pharma amid U.S. drug tariff plans’
- by Lee, Jeong-Hwan Oct 29, 2025 06:10am
- The Ministry of Health and Welfare (MOHW) has pledged to strengthen support measures for Korean pharmaceutical and biotech companies potentially impacted by the U.S. Trump administration's drug tariff policy. However, no specific policies or systems have been announced yet. The government plans to respond once the details of the U.S. administration's proposed drug tariff measures are announced. The MOHW also stated it is implementing various budget projects to foster and localize the materials, parts, and equipment (MPE) industry, which includes active pharmaceutical ingredients for biopharmaceuticals. This information comes from reviewing the Ministry's response submitted to the National Assembly's Health and Welfare Committee on the 27th for its NA audit. In response to concerns over potential damage from the U.S. plan to impose 100% tariffs on pharmaceuticals, the ministry said, “We will expand measures to strengthen export competitiveness, including financial support and new market development for affected companies.” The ministry explained that while President Trump mentioned plans for a 100% drug tariff, no official government announcement specifying the scope or items subject to the tariff has been made yet. The ministry elaborated, “If high tariffs are imposed, it will inevitably impact exports to the U.S. by domestic pharmaceutical and biotech companies. We need to confirm the details of the U.S. administration's specific drug tariff announcement.” It further announced, “The Ministry of Health and Welfare, together with the Ministry of Trade, Industry and Energy, held an emergency meeting with export companies on September 29 regarding the announcement of pharmaceutical tariffs to gather industry opinions. We will strengthen countermeasures for companies affected by tariffs in the biohealth sector to minimize the impact on domestic companies.” Regarding plans to foster the bio-materials and equipment sector as the “second semiconductor MPE” industry, the ministry emphasized that “this holds high importance from a national health security perspective.” The ministry stated it is supporting companies with costs for performance evaluations, such as testing, analysis, and certification, as well as consulting for overseas approvals, to promote the domestic production of vaccines and raw materials, which Korea is currently heavily import-dependent. For 2024, KRW 2.1 billion was allocated to support performance testing of domestically produced vaccine APIs. The ministry also announced new initiatives for the next year, pledging to continue nurturing the bio-materials and equipment sector. “The government's plan for next year includes new projects for the domestic production of bio raw materials and components, reflecting our ongoing commitment to fostering the bio MPE industry. We will provide support through budgeted projects, including KRW 10 billion for stabilizing the supply of bio raw materials and components, KRW 1.5 billion for diversifying raw material procurement, KRW 500 million for stockpiling essential medicines, and KRW 8.1 billion for advancing the manufacturing of export-oriented pharmaceuticals.”
- Policy
- HIRA “Low-price drug incentive brings ₩2.7 savings'
- by Lee, Jeong-Hwan Oct 29, 2025 06:10am
- The Health Insurance Review and Assessment Service (HIRA) defended its position regarding the argument against the ‘low-price drug purchase incentive’ payment system, stating that the system has consistently contributed to national health insurance cost savings. However, it acknowledged that improvements are needed regarding the unresolved issue of incentives being disproportionately concentrated on medical institutions at the general hospital and tertiary hospitals. HIRA's policy is to expand the cost-saving effect on the health insurance budget by devising a plan to allow hospital-level medical institutions and primary care clinics to participate in the low-price drug purchase incentive system. On the 26th, HIRA disclosed this plan regarding the low-price purchase incentive to the office of Representative Joo-young Lee of the Reform Party, Rep Lee raised concerns about the systemic contradictions and low effectiveness of the low-price drug purchase incentive policy. The low drug price purchase incentive system provides incentives to medical institutions based on the difference between the actual purchase price of drugs and the upper limit set for drug costs. Ultimately, this policy incentivizes lowering the actual transaction price of drugs in the market relative to the NHI drug price ceiling. This directly leads to reductions in the actual transaction prices of drugs, affecting pharmaceutical companies' cash cows. Rep Lee believes this incentive system hinders the development of the domestic pharmaceutical industry and diminishes the cost-saving effects of the national health insurance program because it focuses on price rather than drug quality. The pharmaceutical industry and drug wholesalers also argue that the low-price purchase incentive system is inherently flawed because it is linked to reductions in the actual transaction price of drugs. Critics argue that the lower the actual transaction drug price becomes for low-price purchase incentives, the more directly it leads to subsequent reductions in actual transaction drug prices, discouraging all from voluntarily lowering drug prices. Medical institutions have long pointed out that for small and medium-sized hospitals, neighborhood clinics, and pharmacies—not tertiary hospitals—the actual volume of low-price purchases is small, resulting in a low perceived incentive effect. In response to Rep. Lee's criticism that the low-price purchase incentive system is ineffective and undermines drug quality, HIRA stated, “It has the effect of reducing national health insurance finances.” HIRA explained that the low-price purchase incentive program was introduced to motivate healthcare institutions to purchase low-priced drugs and manage drug costs appropriately. It further elaborated, “The financial savings effect through this system is being sustained, as evidenced by the steady influx of new institutions participating in each round.” In fact, new institutions accounted for an average of 31.5% of all institutions receiving low-price purchase incentives recently. The low-price purchase incentive program has reduced national medical expenses by KRW 2.7012 trillion over the past decade, yielding annual savings of approximately KRW 200 to 300 billion. While recognizing the financial benefits, HIRA also admitted that the incentives are concentrated on medical institutions at the general hospital level or above, noting that improvement is needed to ensure fairer participation. HIRA concluded, “Since institutions with strong purchasing power, such as general hospitals, receive most of the incentives, we will seek ways to encourage participation from smaller hospitals and clinics, thereby contributing to the appropriate management of drug costs in Korea.”
- Policy
- How did CPAC evaluate Wegovy's adolescent indication?
- by Lee, Tak-Sun Oct 28, 2025 06:13am
- The Ministry of Food and Drug Safety (MFDS)'s Central Pharmaceutical Affairs Council (CPAC) meeting report on the approval of Wegovy (semaglutide, Novo Nordisk) for a 12-and-above adolescent indication has been released, garnering attention. While CPAC members generally acknowledged the need for the adolescent obesity indication for Wegovy, they agreed that stringent post-marketing safety monitoring is required. The MFDS recently added Wegovy's indication for use as an adjunct to chronic weight management in adolescents aged 12 and older. Wegovy can now be used for obese adolescent patients aged 12 or older with an initial Body Mass Index (BMI) corresponding to the adult threshold of 30 kg/m2 or higher, and whose body weight exceeds 60 kg. The CPAC advisory report, held on July 24, was released on that day. Nine of the twelve members who attended the meeting unanimously agreed on the validity of the efficacy and safety for the adolescent obesity indication. One member stated, "Although there are concerns about misuse and abuse, this is a necessary drug for severely obese adolescents." Another member said, "The adverse events for the GLP agonist class will likely be similar," adding, "Obesity is a disease, and as it is expected to increase, there is a medical necessity." The consensus favored the benefits to patients outweighing concerns about misuse. Another member noted, "While the adult indication includes overweight patients with comorbidities, the adolescent indication is limited to obese patients, which suggests the risk of misuse and abuse might be lower than in adults. However, thorough management in clinical settings appears necessary." Consequently, the MFDS stated it would review the suggestion to include warnings about suicidal ideation in the drug's approval information. In fact, warnings regarding suicidal ideation have been included in the precautions for use. A clause was added to the general precautions stating: "Suicidal behavior and ideation have been reported in clinical trials of other medicines for the treatment of obesity or overweight. Patients receiving this drug for chronic weight management must be monitored for the emergence or worsening of depression, suicidal ideation or behavior, and/or any abnormal changes in mood or behavior. Use of this drug should be discontinued in patients who experience suicidal ideation or behavior. This drug should not be used in patients with a history of suicidal behavior or active suicidal ideation." Furthermore, a plan for post-marketing surveillance (PMS) in adolescents was also approved. The expansion of Wegovy's adolescent indication was primarily driven by the STEP TEENS Phase 3 clinical study. Thiswas a multi-center, randomized, double-blind study involving 201 adolescents aged 12 to less than 18 who were obese or overweight with at least one weight-related comorbidity. The clinical results met the primary endpoint. The percentage change in BMI showed a 16.1% reduction in the Wegovy 2.4mg group (134 patients), compared to a 0.6% increase in the placebo group (67 patients). The percentage of patients achieving 5% or more weight loss, a secondary confirmatory endpoint, was higher in the Wegovy 2.4 mg group (72.5%) compared to the placebo group (17.7%). Additionally, the secondary exploratory endpoint of weight change (kg) showed a 15.3 kg decrease in the Wegovy 2.4 mg group, compared to a 2.4 kg increase in the placebo group. The proportion of patients achieving 15% or more weight loss was also higher in the Wegovy 2.4 mg group (53.4%) than in the placebo group(4.8%). Novo Nordisk Korea stated, "Wegovy is the first GLP-1-based, once-weekly obesity treatment to be approved for adolescents," stressing that it "will improve treatment access for adolescents."
- Company
- Fruzaqla expands its role to late-stage colorectal cancer
- by Son, Hyung Min Oct 28, 2025 06:12am
- A new treatment option has been added to the field of metastatic colorectal cancer, which is classified as a refractory condition. Takeda Korea held a press conference on the 27th at the Plaza Hotel in Jung-gu, Seoul, to commemorate the expanded indication of its colorectal cancer drug, Fruzaqla (fruquintinib). Approved in March as a fourth-line therapy, Fruzaqla was approved to extend its indication as a third-line treatment within just 6 months, becoming one of the key success cases of the Ministry of Food and Drug Safety’s fast-track program (Global Innovative drugs on Fast Track). Clinical evidence for Fruzaqla was established through the global Phase III FRESCO trial involving 416 patients with metastatic colorectal cancer. Results showed the median overall survival (OS) in the Fruzaqla group was 9.3 months, extending survival by 2.7 months compared to 6.6 months in the placebo group. The risk of death decreased by 35%, and adverse events were mostly predictable or manageable. Professor Dong-Hoe Koo of the Department of Medical Oncology at Kangbuk Samsung Hospital These results were published in major international journals such as The New England Journal of Medicine (NEJM) and subsequently recommended as Category 2A in the NCCN Guidelines and Grade I, A in the European Society for Medical Oncology (ESMO) guidelines. Professor Dong-Hoe Koo of the Department of Medical Oncology at Kangbuk Samsung Hospital stated, "Fruzaqla has high drug specificity as it does not target unnecessary targets. This enables efficient VEGFR inhibition and sustained drug exposure. Its potential for combination therapy with existing agents is also worth exploring in future clinical studies.“ He further stated, ”The survival benefit of existing treatments had not been substantial compared to the untreated group. Fruzaqla has shown real-world efficacy comparable to clinical trials, suggesting broader clinical utility.” Still high unmet need...“Expectations for improved survival in late-stage patients” South Korea's colorectal cancer incidence rate was 61.1 per 100,000 population in 2022, the second highest after thyroid cancer. Particularly concerning is the incidence rate among individuals under 40, which reached 12.9 per 100,000, the highest in the world. Colorectal cancer is a malignant tumor that develops in the colon or rectum, classified as colon cancer or rectal cancer based on location. Metastatic colorectal cancer refers to tumors that have spread beyond the primary site to other organs. Because the liver is where blood and lymph from the colon converge, it is the most common site of metastasis, and liver metastasis ranks among the leading causes of death in colorectal cancer patients. However, treatment options remain limited compared to other cancer types. Professor Myung-ah Lee of the Department of Medical Oncology at Seoul St. Mary Currently, in metastatic colorectal cancer treatment, after the first-line therapy ‘Nexavar (sorafenib)’ by Bayer, the standard second-line therapies primarily involve ‘Stivarga (regorafenib)’ by Bayer and ‘Avastin (bevacizumab)’ by Roche in combination with Lonsurf (trifluridine/tipiracil) by Taiho Pharmaceutical in Japan. However, as treatment options beyond the third line have been limited, Fruzaqla’ is expected to play a significant role in the treatment space. Professor Myung-ah Lee of the Department of Medical Oncology at Seoul St. Mary's Hospital stated, “Although several novel targeted therapies have emerged, treatment options remain insufficient beyond the third line. Due to the lack of expected efficacy, the difference in survival benefit has been minimal. Stivarga and Lonsurf have not demonstrated the expected level of effectiveness.” “Patients undergoing third-line or later treatment have already been exposed to numerous anticancer drugs, leading to a diminished quality of life. This is largely linked to the toxicity issues of these drugs. For instance, despite being a targeted therapy, Stivarga had a high incidence of adverse reactions that negatively impact quality of life. Given the shortage of drugs that are both less toxic and effective, Fruzaqla is expected to play a greater role.”
- Company
- Hanmi "Phase 3 trial confirms efficacy of GLP-1 drug"
- by Cha, Jihyun Oct 28, 2025 06:11am
- Efpeglenatide is a GLP-1 drug using Hanmi Pharmaceutical Hanmi Pharmaceutical announced on October 27 that its glucagon-like peptide-1 (GLP-1) obesity treatment candidate, 'HM11260C' (efpeglenatide), met primary endpoints in a Phase 3 top-line study in Korea. The results confirmed significant weight-loss efficacy and safety compared with placebo. This Phase 3 trial involved 448 non-diabetic adult patients with obesity. The study aimed to evaluate the superiority of efpeglenatide over placebo in terms of the mean percentage change in body weight and the percentage of subjects achieving 5% weight loss at 40 weeks. According to Hanmi Pharmaceutical, the 40-week analysis showed a statistically significant difference against placebo. The proportion of subjects achieving 5% weight loss was 79.42% in the efpeglenatide group versus 14.49% in the placebo group. The mean percent weight change was -9.75% in the efpeglenatide group versus -0.95% in the placebo group, confirming a least-squares mean difference of -8.13% between the groups. In terms of safety, gastrointestinal adverse events were reported but generally manageable: nausea 16.72% (5.37% with placebo), vomiting 11.71% (2.01% with placebo), and diarrhea 17.73% (4.70% with placebo). Hanmi Pharmaceutical plans to apply for marketing authorization with the Ministry of Food and Drug Safety (MFDS) for efpeglenatide within this year. The company explained, "Although the clinical trial involves dosing and observation up to 64 weeks, we are disclosing the 40-week interim top-line data with a plan for a submission within the year," and added, "We expect to derive improved indicators from continued dosing beyond the data announced now." Efpeglenatide is a GLP-1 drug using Hanmi Pharmaceutical's long-acting platform, 'LAPSCOVERY,' and is the most advanced clinical-stage candidate in the company's obesity and metabolic disease pipeline. It is also the fastest-developing obesity treatment among domestic Korean companies. Hanmi Pharmaceutical initially out-licensed efpeglenatide to Sanofi for diabetes in 2015 for up to €3.9 billion (approximately KRW 5.597 trillion). However, Sanofi returned the rights to the pipeline in June 2020, citing a change in business strategy. In 2023, Hanmi Pharmaceutical officially announced its decision to develop efpeglenatide, initially developed for diabetes, as an obesity treatment, mirroring the strategies of Novo Nordisk and Eli Lilly in repurposing their diabetes drugs. The core of Hanmi's strategy is the creation of a 'Korean GLP-1 Obesity Drug'. The company intends to develop efpeglenatide as a GLP-1 obesity treatment tailored to the characteristics of the Korean obese population, which has a lower proportion of severely obese patients. In a global market where Novo Nordisk and Eli Lilly have established overwhelming dominance, Hanmi Pharmaceutical aims to differentiate through price competitiveness and a stable supply chain. Kim Na-young, Executive Director of Hanmi Pharmaceutical's New Product Development Division, who led the study, stated, "Efpeglenatide, a drug the late founder of Hanmi Group, Lim Sung-ki, was passionate about, has taken a big step toward commercialization as a 'national obesity drug' by yielding effective and safe clinical results in a Korean population study," and concluded, "Efpeglenatide will become a new drug demonstrating diverse potential in the metabolic disease sector, spanning from obesity to diabetes."
- Opinion
- [Reporter’s View] China’s rise poses new challenges
- by Hwang, byoung woo Oct 28, 2025 06:11am
- One of the most striking features at the European Society for Medical Oncology (ESMO 2025) Congress in Berlin, Germany, was the clear rise of China. Chinese researchers’ names appeared repeatedly across major sessions, and the word “China” was visible throughout the poster halls. Compared to previous years, more Chinese companies submitted abstracts, with some securing spots not only in ‘Late-breaking Abstract (LBA)’ presentations but also in the prestigious Presidential sessions, ESMO's highest-level presentations. This was a scene rarely seen at global conferences just a few years ago. Particularly noteworthy is that despite most corresponding authors and key speakers of major abstracts being Chinese researchers, they were included in core sessions, underscoring the growing recognition and expectation for Chinese innovation in oncology. Consequently, the ESMO 2025 press room saw a greater-than-usual number of Chinese journalists visiting for coverage. A representative case was the Phase III study on sacituzumab tirumotecan (Sac-TMT), an antibody-drug conjugate (ADC) jointly developed by Kelun-Biotech and Merck. In particular, China is leading a large number of next-generation modality studies, including antibody-drug conjugates (ADCs), bispecific antibodies, and immune-oncology combination therapies. Industry experts at the scene said that China has evolved from being a ‘fast follower’ to becoming a ‘fast mover.’ This transformation is underpinned by government support, substantial capital, and a rapid clinical system. China's regulatory, clinical, and investment ecosystems are organically integrated, with global development taken into account from the earliest candidate stage. The short turnaround between clinical registration and publication has become a competitive advantage. Of course, the sheer scale of China’s domestic market cannot be ignored. However, considering the recent wave of Chinese new drug data being presented at major academic conferences, the prevailing view is that it is no longer feasible to dismiss this as merely ‘for local use’. It's not that Korean companies haven't produced meaningful data. Some garnered attention with novel mechanisms and technologies, but the issues lie in speed and scale. The gap with China was evident in the number of publications, the depth of clinical stages, and global expansion capabilities. A researcher at the conference stated, “Even with promising candidates, the journey to clinical trials and approval is too slow. China is already opening institutional pathways at the national level.” The challenge for Korea’s pharma industry is clear: while scientific foundations are strong, the sector must overcome constraints in capital and manpower that are required to scale this into clinical development.. The direction for Korea to take is already being demonstrated by some companies. There has been an increase in cases where overseas clinical trials and regulatory approval processes are designed together from the initial stages, and platform-focused research, such as ADCs and bispecific antibodies, is also expanding. However, it is difficult to say that this strategy has spread across the entire industry. Clinical trials prioritizing domestic approval and single-candidate-focused development still dominate. Global design in new drug development is no longer a foreign concept in Korea. Many companies are designing overseas clinical trials and regulatory approval processes from the initial stages, keeping global expansion in mind. However, it is difficult to say that this strategy has become established across the entire industry. Clinical trials primarily targeting domestic approval and development centered on single candidates still constitute a significant portion. To compete globally, Korea must strengthen platform-based scalability, clinical design capabilities, and the talent ecosystem that supports both. The government, too, must move beyond short-term project funding and establish a strategic system that integrates global clinical development with regulatory reform. The pace of China’s progress, as this reporter felt in Berlin, is not merely in the sheer volume of research. It stemmed from a fundamental difference in the structure of the entire industry. Drug development is no longer a contest of ideas but of systems. If Korea’s government continues to highlight biopharma as a national growth engine yet fails to keep pace with this shift, the country risks being relegated to the role of a spectator in the global pharmaceutical arena.