- LOGIN
- MemberShip
- 2025-12-19 07:23:56
- Policy
- NA requests rapid reimb listing for diabetes drug Mounjaro
- by Jung, Heung-Jun Nov 11, 2025 06:08am
- The Ministry of Health and Welfare (MOHW) announced that it will reflect the results of the October expert advisory meeting in reimbursement criteria for Mounjaro (tirzepatide), Eli Lilly’s dual GIP/GLP-1 receptor agonist, following growing calls for its rapid inclusion under the National Health Insurance for type 2 diabetes. The ministry also stated it is working to ensure the smooth reimbursement process for Ozempic (semaglutide), Novo Nordisk’s GLP-1 receptor agonist, which was reviewed by the Drug Reimbursement Evaluation Committee in October. On the 10th, Miae Kim, a lawmaker from the People Power Party, inquired about the current status of the reimbursement application process for Mounjaro for type 2 diabetes during a written inquiry session for the Ministry of Health and Welfare's comprehensive audit. She also questioned the plans for utilizing the expedited listing system, which reflects international drug prices and reimbursement cases. According to the Ministry of Health and Welfare, Mounjaro applied for reimbursement approval in March last year and was discussed by the Drug Reimbursement Criteria Subcommittee in May of the same year. Subsequent evaluations on its reimbursement adequacy were conducted in August and December 2023, and March and June 2024 by the Cost-Effectiveness Evaluation Subcommittee. The Ministry explained, “The company applied for reimbursement of Mounjaro in March last year and is currently undergoing a review on its reimbursement adequacy. The drug is being reviewed in accordance with HIRA regulations, referencing factors such as its listing status in other countries, listed prices, and coverage criteria.” It added, “To ensure appropriate use of the GLP-1 agonists Mounjaro and Ozempic for diabetes patients, HIRA held an expert advisory meeting last October to discuss patient selection criteria and evaluation methods. The findings will be reflected in the drug's reimbursement criteria.” Rep. Seo Mi-hwa of the Democratic Party of Korea also inquired about the Ministry's stance on reviewing insurance coverage for new drugs to strengthen diabetes management. The Ministry responded, “We agree that the health insurance coverage of new diabetes drugs should be actively reviewed. Currently, GLP-1 receptor agonists Ozempic and Mounjaro are undergoing the listing process. We will closely monitor to ensure the listing process proceeds smoothly and continue our efforts to improve treatment accessibility.”
- Company
- Yuhan-Janssen Korea to jointly sell 'Leclaza + Rybrevant'
- by Son, Hyung Min Nov 11, 2025 06:08am
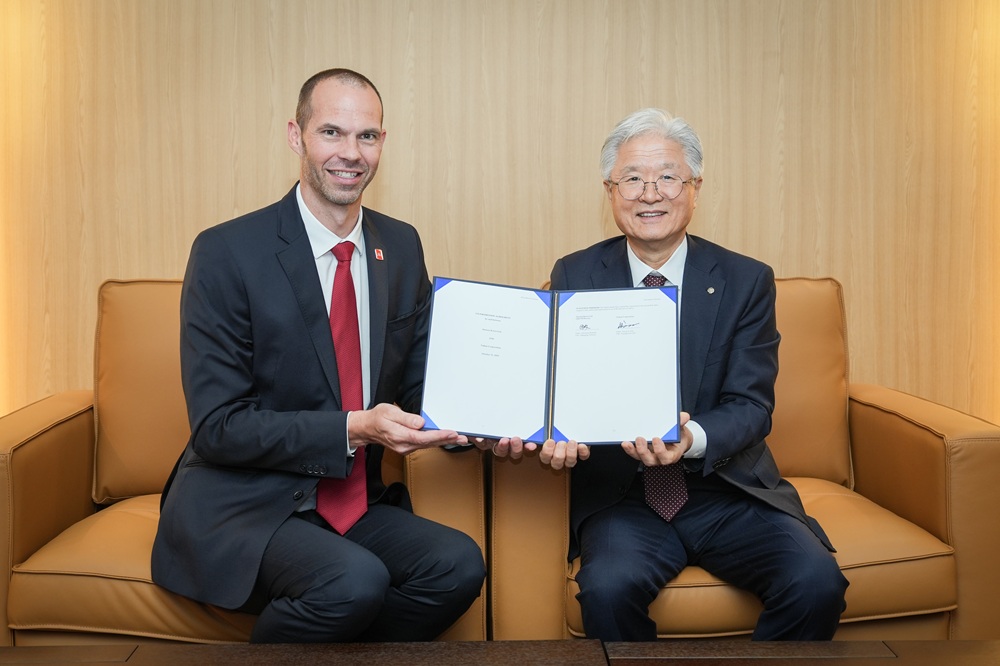
- (from left) Christian Rodseth, Managing Director of North Asia for Johnson & Johnson Johnson & Johnson's Korea-based pharmaceutical unit, Janssen Korea (CEO Chris Rodseth), announced that it will jointly conduct domestic promotion for the non-small cell lung cancer treatment combination therapy, Leclaza (lazertinib) + Rybrevant (amivantamab), with Yuhan Corporation (Yuhan). Previously, promotional activities for the Leclaza + Rybrevant combination therapy were led by Johnson & Johnson, which holds the global rights. Through this new agreement, the promotion will be conducted jointly with Yuhan. Yuhan had previously been responsible for promoting Leclaza monotherapy and will now expand its role to include co-promotion of the combination therapy. The Leclaza + Rybrevant combination therapy received approval from the Ministry of Food and Drug Safety (MFDS) this January for the first-line treatment of non-small cell lung cancer (NSCLC) with EGFR exon 19 deletions or exon 21 (L858R) substitution mutations. Christian Rodseth, Managing Director of North Asia for Johnson & Johnson's pharmaceutical sector, said, "Through this strategic partnership with Yuhan, we hope that more NSCLC patients in Korea can benefit from the treatment of this combination therapy." Rodseth added, "Johnson & Johnson is dedicated to changing patients' lives through science and innovation, and we will do our best to provide better treatment opportunities to patients based on close collaboration and communication with Yuhan." In addition to Leclaza monotherapy, for which Yuhan holds the rights and conducts promotion in Korea, Johnson & Johnson will exclusively conduct promotion for: second-line or later treatment of adult NSCLC patients with EGFR exon 19 deletion or exon 21 (L858R) substitution mutations, and first-line treatment of adult NSCLC patients with EGFR exon 20 insertion mutations. Johnson & Johnson will also supply Rybrevant exclusively.
- Company
- NSCLC standard treatment options undergo major change
- by Son, Hyung Min Nov 11, 2025 06:07am
- YuhanThe Leclaza + Rybrevant combination therapy has been recommended as the first-line treatment option by the National Comprehensive Cancer Network (NCCN) guidelines, based on its clinical utility. With Tagrisso also listed as a preferred therapy in combination with platinum-based chemotherapy, combination therapy is expected to become the major strategy in first-line treatment for EGFR-positive non-small cell lung cancer (NSCLC). According to industry sources on November 8, the NCCN recently revised its NSCLC treatment guidelines, including the combination of Yuhan's 'Leclaza (lazertinib)' and Janssen's 'Rybrevant (amivantamab)' as a Category 1 Preferred, first-line recommendation for EGFR-positive NSCLC. Consequently, experts preferentially recommend combination therapy as first-line treatment when an EGFR exon 19 or exon 21 mutation is identified in NSCLC. The Leclaza + Rybrevant combination therapy, which was first listed as a general recommendation last year, achieved the significant result of being changed to a Preferred recommendation in just about a year. This opens the door to recognition of combination therapy as a Standard of Care (SOC) globally. The NCCN provides guidelines for the diagnosis, treatment, and prognosis of cancer. This organization is a federation of 32 institutions, including U.S. National Cancer Centers and research institutes, and healthcare professionals worldwide refer to NCCN as a primary guide for cancer care and treatment. The reason the Leclaza + Rybrevant combination therapy was listed as a Preferred recommendation by the NCCN is that it secured sufficient efficacy results. Leclaza is a new EGFR-positive NSCLC drug developed by Yuhan, a 3rd-generation tyrosine kinase inhibitor (TKI) targeting exon 19 and exon 21 (L858R) mutations. Johnson & Johnson secured the global rights to Leclaza and has been conducting clinical research to evaluate its efficacy in combination with Rybrevant, a targeted treatment option that targets exon 20 and the MET mutation. The final overall survival (OS) analysis of the Leclaza + Rybrevant combination therapy showed superior OS compared to 'Tagrisso (osimertinib)' monotherapy. This combination therapy is currently expected to secure the longest OS results among all pivotal clinical studies for EGFR-positive targeted therapies. In the trial, the combination therapy group showed a statistically significant improvement in survival compared with the Tagrisso monotherapy group (p< 0.005). In detail, the median OS for the Leclaza + Rybrevant group was not estimable (42.9 months-NE). In contrast, the Tagrisso group showed an OS of 36.7 months. Based on the distribution of survival indices, the Leclaza + Rybrevant group is expected to extend OS by at least 12 months compared with the Tagrisso group. These study results were recently published in the New England Journal of Medicine (NEJM), attracting significant attention from the academic community. Previously, Tagrisso monotherapy, a 3rd-generation TKI targeting EGFR exons 19 or 21, had been recommended as the Preferred treatment option in major guidelines, such as the NCCN guidelines. However, the Leclaza + Rybrevant combination therapy, which is a 3rd-generation TKI similar to Tagrisso, demonstrated superior results compared to Tagrisso monotherapy, suggesting potential changes in key cancer treatment guidelines. The Leclaza + Rybrevant combination therapy is achieving significant success in both the OS results, which were identified as the key to commercialization, and its NCCN guideline listing. As the NCCN guidelines have been revised, the Leclaza + Rybrevant combination therapy has been recommended as the first-line treatment option. Tagrisso + platinum-based chemotherapy receives the priority recommendation…combination with Rybrevant possible AstraZenecaTagrisso was also recommended as a preferred therapy in combination with platinum-based chemotherapy, alongside its monotherapy use. While Tagrisso became the SOC for first-line EGFR-positive NSCLC through monotherapy, the Leclaza + Rybrevant combination therapy joined the competition. AstraZeneca received approval for Tagrisso in combination with platinum-based chemotherapy as a first-line EGFR-positive treatment. The company aims to extend survival by using chemotherapy, previously a second-line treatment, at an earlier stage. The Tagrisso + platinum-based chemotherapy combination therapy demonstrated efficacy compared with Tagrisso monotherapy in the FLAURA2 study. The clinical results showed that the combination therapy recorded an OS of 47.5 months, longer than Tagrisso monotherapy's 37.6 months. The median Progression-Free Survival (PFS) based on the investigators' assessment was 25.5 months, an extension of 8.8 months compared with Tagrisso monotherapy at 16.7 months. AstraZeneca is confirming the possibility of combining its targeted therapies with various options. The company is currently conducting combination trials of Tagrisso with the Antibody-Drug Conjugate (ADC) 'Datroway (datopotamab)' and the targeted therapy 'savolitinib'. In addition, AstraZeneca is conducting a clinical trial in collaboration with the global Contract Research Organization (CRO) Parexel to assess the combination potential of Tagrisso and Rybrevant. The Phase 2 OSTARA study began in July 2023 and is evaluating the efficacy and safety of the Tagrisso + Rybrevant combination therapy as a first-line treatment for EGFR-positive NSCLC. With the efficacy of the Rybrevant + Leclaza combination therapy validated, AstraZeneca also plans to confirm the potential of combining Tagrisso with a targeted therapy.
- Policy
- Cancer & orphan drugs apply for reimb within 1 week of apv
- by Jung, Heung-Jun Nov 10, 2025 06:10am
- Anticancer drugs and rare disease drugs that were approved in Korea this year are racing to apply for reimbursement as quickly as within a week. Six rare/serious disease treatments approved by the Ministry of Food and Drug Safety this year are undergoing reimbursement review, excluding those subject to the approval-evaluation-negotiation system. According to industry sources on the 7th, multiple new drugs, including those designated under the Global Innovative product on Fast-Track (GIFT) scheme, are applying for reimbursement quickly after approval. Takeda Korea’s Fruzaqla (fruquintinib), which was approved in March for metastatic colorectal cancer, was submitted for reimbursement last month and is currently being assessed for clinical benefit. The drug, designated GIFT No. 20, was specifically requested for expedited coverage during this year’s NA MOHW audit as a third-line therapy for metastatic colorectal cancer. Qalsody (tofersen), Biogen’s amyotrophic lateral sclerosis (ALS) treatment and GIFT No. 31, received approval on August 20 and was immediately filed for reimbursement to expand its prescription. Imdelltra (tarlatamab), Amgen Korea’s small-cell lung-cancer drug (GIFT No. 25), was approved on May 30 and submitted for reimbursement on August 28. Augtyro (repoterrectinib), Bristol Myers Squibb’s therapy for metastatic non-small-cell lung cancer and solid tumors, followed a similar path — approved in June, filed 2 months later. Gilead Sciences’ Yescarta (axicabtagene ciloleucel), a CAR-T therapy for diffuse large B-cell lymphoma, and Janssen Korea’s Opsynvi (macitentan + tadalafil) for pulmonary arterial hypertension, both received approval in July and August, respectively, and each applied for reimbursement within just 1 week of approval. Opsynvi is now undergoing a cost-effectiveness evaluation. Industry analysts attribute this accelerated pace partly to the current administration’s policy direction under President Jae-myung Lee, which emphasizes improving patient access to orphan and severe-disease treatments. However, even with early reimbursement filings, such drugs typically face lengthy review cycles as significant time is required for clinical utility and cost-effectiveness reviews. Even if they clear the threshold of proof, a protracted drug price negotiation process remains. Currently, 33 drugs that applied for reimbursement last year and this year remain under review, suggesting fierce behind-the-scenes competition among drugs for priority listing.
- Company
- HAE treatment 'Takhzyro' closer to reimbursement
- by Eo, Yun-Ho Nov 10, 2025 06:08am
- Product photo of Takhzyro (lanadelumab) A hereditary angioedema (HAE) treatment, 'Takhzyro,' appears closer to insurance reimbursement listing, approximately five years after acquiring domestic approval in South Korea. Takeda Korea's Takhzyro (lanadelumab) has recently passed the Drug Reimbursement Evaluation Committee (DREC). This is the first achievement since receiving approval from the Ministry of Food and Drug Safety (MFDS) in February 2021. Attention has been drawn to whether Takhzyro will successfully undergo drug pricing negotiations with the National Health Insurance Service (NHIS) to become a new treatment option for the HAE area, where treatments are lacking. HAE is a rare disorder caused by dysfunction of the C1-esterase inhibitor (C1-INH) protein, resulting in recurrent, unpredictable, and sudden swelling in different parts of the body. Upper airway edema can restrict breathing and lead to asphyxiation. Gastrointestinal tract swelling can cause emergency events, such as severe pain and intestinal obstruction. Approximately 40% of patients have their first episode before age 5, and 75% before age 15. However, most individuals undergo a 'diagnostic odyssey' and receive an accurate diagnosis only as adults. This is why the number of diagnosed cases in South Korea was only 200-250 as of last year, despite an estimated total of approximately 1,000 patients. In fact, it takes an average of 19 years to get diagnosed. Even after the diagnosis, patients are exposed to unpredictable HAE attacks and emergencies. However, in South Korea, patient access to treatments that provide fundamental care has been low. Therefore, the medical field has been consistently requesting reimbursement listing for Takhzyro. It remains to be seen whether drug price negotiations with the NHIS for Takhzyro will be successfully concluded and emerge as a new treatment option for HAE, where therapeutic agents are scarce. Meanwhile, Takhzyro demonstrated efficacy in the Phase 3 HELP study. The study results showed that the group receiving Takhzyro every two weeks reduced the average monthly attack frequency of HAE attacks by 87% compared with the placebo group, while the group receiving Takhzyro every four weeks achieved a 74% reduction.
- Policy
- Budget cut 20% despite increased COVID-19 vaccine uptake
- by Lee, Jeong-Hwan Nov 10, 2025 06:08am
- The Korea Disease Control and Prevention Agency (KDCA) has cut the national immunization program (NIP) budget for COVID-19 vaccines for the 2026-27 season by 20% compared to the previous year, raising societal concern over potential drops in immunity among high-risk groups like the elderly, increased mortality risk, and the possibility of early vaccine stock depletion. Moreover, the KDCA’s 20% cut to the COVID-19 NIP budget was based on the 2023-2024 season's vaccination rate of 42%, failing to reflect the 48% rate from this season (2024-2025 season). This has drawn criticism as an administrative decision that undermines effective epidemic prevention. The National Assembly Budget Office pointed out that both the number of vaccinated individuals and the coverage rate are on the rise, and has urged the KDCA to raise its target vaccination rate and revise the budget accordingly. The Budget Office recommends increasing the budget from the government’s draft of KRW 175.8 billion to KRW 200.8 billion – a KRW 25 billion increase. On the 10th, the National Assembly Health and Welfare Committee will review the KDCA budget, including the COVID-19 vaccine NIP budget, during its plenary session. The COVID-19 vaccine NIP covers high-risk groups - persons aged 65 and older, residents in communal or institutional facilities aged 6 months to 64 years, and immunocompromised individuals – with the aim of securing immunity and preventing severe illness and death. The KDCA set the 2026 NIP budget based on a vaccination rate of 42%. But looking at recent seasons, the number vaccinated was 2.90 million (39.3%) in 2022-23; 4.10 million (41.3%) in 2023-24; and 4.97 million (47.8%) in 2024-25, it was for the 65+ age group, continuing an upward trend. The major issue highlighted by experts and the Budget Office was that, despite rising vaccine uptake, the KDCA’s budget estimate remains anchored to the 42% figure from the 2023-24 season. Given statistics showing the 2024-2025 season vaccination rate approaching 48%, experts and the Office believe that setting the budget based on an incorrect baseline will inevitably lead to early vaccine depletion if the vaccination levels stay the same or increase, making it impossible to achieve the target vaccination rate. The argument is that recognizing the vaccine budget as an investment rather than an expense and rationally increasing the budget for infectious disease response is necessary to prevent potential outbreaks among high-risk groups and increases in mortality rates. In fact, 5.3 million doses of COVID-19 vaccines were secured this year based on last year's vaccination rate. However, increased uptake due to simultaneous COVID-19 and flu vaccination campaigns by health authorities and local governments led to vaccine shortages at some medical institutions just 2 weeks after the National Immunization Program (NIP) began. The NIP is a public health investment to protect citizens' lives. Prioritizing long-term effects over short-term costs will lead to socioeconomic benefits, including reduced healthcare expenses, alleviated burden on the medical system, and maintained national productivity. Furthermore, since the 2023 declaration of endemic status, COVID-19 has continued to mutate repeatedly, with the number of hospitalized patients and mortality rates constantly being reported. According to the KDCA’s infectious disease portal sample surveillance results, the number of COVID-19 hospitalizations last year was approximately 3 times that of influenza hospitalizations. The mortality rate was also higher for COVID-19 hospitalized patients at 5.97%, compared to 3.75% for influenza hospitalized patients. In the National Assembly, lawmakers, including Representative Jin-sook Jeon and Representative Nam-hee Kim of the Democratic Party of Korea, have been scrutinizing the KDCA's unreasonable NIP budget cuts. In response, the NA Budget and Planning Office has proposed the need to increase next year's NIP budget to reflect the rising trend in COVID-19 vaccination numbers and rates. The request is to increase the budget by KRW 25 billion, raising it from the KDCA's budget of KRW 175.8 billion (based on a 42% target vaccination rate) to KRW 200.8 billion (based on a 48% vaccination rate). The Budget and Planning Office analyzed, “Considering the recent trend of increasing COVID-19 NIP vaccinated individuals and vaccination rates across all 3 seasons, there seems to be a need to increase the project budget. Calculating the budget based on raising the target vaccination rate from 42% to 48% (a 6 percentage point increase) results in an estimated KRW 200.8 billion, an additional KRW 25 billion .”
- Policy
- ‘No drugs are benefitting from Korea's dual pricing scheme'
- by Jung, Heung-Jun Nov 10, 2025 06:08am
- Although a separate contract system was introduced for dual pricing of drugs in March this year, following a Ministry of Health and Welfare notice, no drugs are currently subject to the dual drug pricing system, prompting the government to review expansion plans. The NHIS stated it is reviewing with the government on expanding the scope of drugs eligible for the separate contract system. On the 7th, Democratic Party of Korea lawmakers Young-seok Seo and Byeong-hoon So submitted written inquiries during the NHIS’s comprehensive NA audit, seeking clarification on the direction and intent behind expanding the dual pricing policy. The Ministry of Health and Welfare had enacted a new notice titled “Evaluation criteria for drugs requiring assessment based on their impact on healthcare” in March, thereby introducing the separate contract system. Rep Young-seok Seo questioned the drugs currently subject to the system and the operational plan. The NHIS responded, “To be subject to the separate contract system, a drug must satisfy all 3 conditions: being an innovative new drug developed by an innovative pharmaceutical company, being approved under the expedited review system, and having undergone domestic clinical trials. Currently, there are no drugs that meet all the criteria. It added, “We are reviewing with the government and other stakeholders the expansion of drugs subject to the separate contract system to facilitate the early introduction of innovative new drugs for patient treatment access.” Representative Byeong-hoon So inquired about plans for expanding the dual pricing system. He also questioned whether plans exist to ensure fiscal stability when expanding the refund-type contract system. The NHIS stated, “Considering the enhancement of health insurance sustainability and the promotion of an innovative industrial ecosystem, we will consult with the government to improve the drug listing system, including expanding the separate contract system, and establish a balanced roadmap.”
- Company
- GSK seeks reimb for self-injectable form of its asthma drug
- by Eo, Yun-Ho Nov 07, 2025 06:17am
- The self-injectable formulation of the antibody drug ‘Nucala’ is aiming to enter Korea’s insurance reimbursement system. GSK Korea recently filed for insurance reimbursement of its Nucala Autoinjector (mepolizumab), an anti-IL-5 (interleukin-5) antibody for treating eosinophilic diseases. Nucala Autoinjector was approved in Korea last March and was released as a non-reimbursed drug this month after securing a distribution network and supply volume. It remains to be seen whether Nucala, which has established its position in the field of eosinophilic asthma, can successfully secure reimbursement coverage for the new formulation upon its launch and expand its influence in Korea. The new autoinjector formulation is approved not only for severe eosinophilic asthma in adults and adolescents (12 years and older), but also ▲ eosinophilic granulomatosis with polyangiitis (EGPA) in adults, and ▲ hypereosinophilic syndrome (HES) in adults. This medication is a self-administered injection used to treat eosinophilic diseases. It is indicated as add-on maintenance therapy in adolescents and adults aged 12 years and older with severe eosinophilic asthma (SEA), as add-on maintenance therapy in adult patients with eosinophilic granulomatosis with polyangiitis (EGPA), and as add-on maintenance therapy in adult patients with hypereosinophilic syndrome (excluding HES, FIP1L1-PDGFRα positive patients). The autoinjector formulation enables patients to self-administer injections conveniently at home. This is evidenced by a self-injection success rate exceeding 96%, high patient preference, and ease of use. Meanwhile, Nucala has been enhancing its competitiveness by securing an indication for chronic obstructive pulmonary disease (COPD). The drug obtained additional approval from the U.S. FDA in May as an “add-on maintenance therapy for adult patients with COPD with an eosinophilic phenotype.” This approval was based on the results of the Phase III MATINEE and METREX studies. In these studies, among a broad spectrum of COPD patients with an eosinophilic phenotype, the Nucala treatment group showed a significantly lower annual rate of moderate-to-severe exacerbations compared to the placebo group.
- Company
- "Rise of regenerative aesthetics focused on natural beauty"
- by Hwang, byoung woo Nov 07, 2025 06:17am
- As the use of medical aesthetics treatments expands, the field is moving away from excessive volume correction toward a focus on natural balance and improved skin quality. As the proportion of surgical procedures decreases, minimally invasive procedures are expanding, and a strategy focused on maintaining long-term safety and efficacy is becoming more critical. DailyPharm met with Dr. Jonathan Kadouch, a dermatologist in the Netherlands, to discuss trends in global medical aesthetics and strategies for safety management in injectable procedures. "From overcorrection to balance...natural aesthetics is trending" Dr. Kadouch explained that the most significant recent change in the field of medical aesthetics is the 'transition from overcorrection to natural harmony.' Dr. Jonathan Kadouch (dermatologist in the Netherlands)"Over the past 20 years, surgical procedures have decreased, and minimally invasive injectable procedures have become the mainstream," he said. "The focus is shifting from simply adding volume to restoring balance, considering the face's structure and tissue changes." Notably, strategies to enhance the skin's inherent quality and its regeneration process are currently gaining attention. Dr. Kadouch said, "Regenerative aesthetics is not just about creating volume, but about creating an environment where tissues can heal themselves," and added, "As interest in regenerative medicine, such as quality improvement, is growing, the medical aesthetics trend is evolving toward prioritizing procedure safety." Dr. Kadouch also emphasized, "In the past, artificially correcting many areas of the face was popular, but now, both patients and medical professionals prioritize natural and long-term sustainable results." "HA and CaHA differ in mechanism and complication management" The major injectable agents are Hyaluronic Acid (HA) fillers and Calcium Hydroxylapatite (CaHA). Although they appear similar, the two agents differ in their mechanisms of action and approaches to managing complications. First, HA fillers are characterized by their degradability with hyaluronidase. This allows for immediate management should side effects occur or if aesthetic adjustments are needed during the procedure. In contrast, CaHA is a microparticle that induces collagen and elastin production as it gradually degrades in the body. Dr. Kadouch distinguished them, explaining, "HA is a natural component of the human body found in joints, eyes, and skin, and has established itself in the medical aesthetics market for improving volume and wrinkles." He added, "CaHA is a biostimulator that promotes tissue regeneration, where anatomical understanding and the precision of the injection layer determine the treatment outcome." Given the high interest in minimally invasive procedures and safety, the approach to managing complications differs between HA and CaHA. Dr. Kadouch explained, "The biggest advantage of HA filler is its reversibility, meaning most issues can be managed by dissolving the filler using hyaluronidase." He noted, "CaHA lacks a dissolving enzyme, requiring an algorithm-based approach to reduce particle concentration or induce tissue diffusion." Dr. Kadouch also mentioned, "The lack of a specific dissolving agent can be a burden for practitioners with limited clinical experience with CaHA. However, as CaHA is increasingly used for regenerative purposes rather than volume correction, the risks of complications and side effects have significantly reduced compared to the past." "Evidence-based product selection and patient expectation management are key" Notably, Dr. Kadouch emphasized that while complications and adverse reactions from filler procedures are often multifactorial, selecting products based on scientific evidence is crucial for ensuring procedure safety. "The more clinical papers and research results a product has accumulated to prove its safety and efficacy, the higher the confidence a practitioner can have in selecting that product," Dr. Kadouch said. "Therefore, rationale decision-making based on objective data and literature is the starting point for safe procedures." Dr. Kadouch said, "Some biostimulator agents have long-proven safety and efficacy," and added, "In contrast, some rapidly expanding new products lack sufficient data accumulation, necessitating a cautious approach." He also explained that with the increase in patients requesting specific procedures seen on social media, the consultation process is important for managing patient expectations. Dr. Kadouch stated, "As information dissemination through social media accelerates, the speed at which specific procedures or products become trends has also become very fast. Combined with new products and marketing, physicians in the medical aesthetics field face greater challenges than before." However, Dr. Kadouch believes that medical professionals must uphold their medical convictions and ethical standards while still meeting patient expectations amid this changing trend. Dr. Kadouch emphasized, "If medical professionals present scientific evidence and logical reasons, many patients understand and prioritize safety in their decisions," and stressed, "Adequately guiding patients on the limitations of expectations and the criteria for safe product selection is essential not only for medical ethics but also for providing trust-based treatment." Finally, Dr. Kadouch projected that the future of the medical aesthetics field will center on improving skin quality, long-term maintenance treatment, and combined-procedure strategies. Dr. Kadouch said, "Across the industry, invasive procedures are being minimized, and the shift toward minimally invasive or non-invasive procedures is clear and expected to continue," and added, "Combining the advantages of different procedures to improve overall skin quality is expected to become the core trend in the aesthetics field."
- Policy
- The application for selective reimb of new drugs is stalled
- by Jung, Heung-Jun Nov 07, 2025 06:17am
- Roche Korea's 'Perjeta (pertuzumab),' a breast cancer treatment, was not on the recent Cancer Disease Review Committee (CDRC) agenda, despite expectations, raising questions about the background of its exclusion. One analysis suggests that the government's policy shift toward strengthening access to rare and severe disease treatments may have contributed. The view is that the Health Insurance Review & Assessment Service (HIRA) must exercise caution in applying selective reimbursement to drugs, as it aligns with impending changes to government policy. According to industry sources on the 5th, discussions on establishing reimbursement criteria for Roche Korea's HER2-positive breast cancer treatment, Perjeta, were not considered in the recent CDRC meeting, reportedly due to an application for selective reimbursement. The CDRC meeting results determined the reimbursement status for 6 products from 5 companies. Perjeta, which was expected to be on the agenda, was not included in the list of drugs discussed. Perjeta is currently applicable for selective reimbursement (with a 30% patient co-payment) for neoadjuvant (pre-operative) therapy for early breast cancer. It is reported that the company has now also applied for selective reimbursement for the post-operative therapy indication. Selective reimbursement was first implemented in 2018 under the previous Moon Jae-in administration as part of its healthcare policy to provide coverage for non-reimbursed treatments. At the time, the government planned a 3-year timeline for anti-cancer drugs and a 5-year timeline for general drugs under the Moon Jae-in Care policy, aiming to reduce patient burden for drugs with high social demand but difficult full reimbursement. With this policy, some new drugs, including anti-cancer agents, received selective reimbursement, but attempts to enter this category have been rare since. Most recent changes involve adjustments to the patient co-payment ratio for drugs already under selective reimbursement. Looking at the current list of reimbursed drugs, 123 items are subject to selective reimbursement. Excluding 97 choline alfoscerate products, which were transitioned to selective reimbursement (with an 80% co-payment) last September, the number of new drugs granted selective reimbursement is small. No new drugs have been granted selective reimbursement this year. The Lee Jae Myung administration is currently pushing a plan to expand access to treatment for rare and severe diseases. Although specific implementation plans have not been formalized, a systemic reform is anticipated. Consequently, analysis suggests that the implementation of selective reimbursement for new drugs, which was part of the previous administration's 3- to 5-year plan, is being delayed to align with the latest, changing policy direction.