- LOGIN
- MemberShip
- 2025-12-21 08:29:26
- Company
- Adstiladrin receives orphan drug designation in Korea
- by Eo, Yun-Ho Jun 18, 2025 05:59am
- The new bladder cancer drug Adstiladrin has been designated as an orphan drug in Korea. The Ministry of Food and Drug Safety recently announced the news in a orphan drug designation announcement. The specific indication for designation is “treatment of BCG-refractory high-risk non-muscle-invasive bladder cancer (NMIBC) with carcinoma in situ (CIS) with or without papilloma.” Adstiladrin (nadofaragene firadenovec-vncg) received FDA approval in the United States in 2022. This drug uses a non-replicating adenovirus vector to deliver the human interferon alpha-2b gene, inducing an immune response by directly expressing the protein within the bladder epithelium. Adstiladrin demonstrated efficacy through the NCT02773849 clinical trial that involved 157 patients with bladder cancer. In the study, 51% of the 98 patients treated with Adstiladrin achieved complete response (CR). The median duration of response was 9.7 months. In addition, 46% of patients who achieved CR remained recurrence-free at 12 months after treatment. The most commonly reported side effects were instillation site discharge (33%), fatigue (24%), bladder spasms (20%), urinary urgency (19%), and hematuria (17%). The rate of discontinuation due to side effects was 1.9%. Non-muscle-invasive bladder cancer (NMIBC) is an early-stage bladder cancer confined to the bladder mucosa, accounting for approximately 70–80% of all bladder cancers. Among these, high-risk patients include those with carcinoma in situ (CIS) or multifocal high-grade tumors, which have a high risk of recurrence and invasion. Although BCG instillation therapy is used as first-line treatment, approximately 30–50% of patients eventually experience recurrence or become resistant within a few months. While radical cystectomy is considered the standard treatment thereafter, as it is a highly invasive surgery, there has been a continued demand for bladder-preserving therapeutic alternatives.
- Company
- Long-acting HIV treatment shifts HIV treatment paradigm
- by Whang, byung-woo Jun 18, 2025 05:59am
- With insurance reimbursement now available for the long-acting HIV (human immunodeficiency virus) treatment Vocabria+Rekambys injection therapy, expectations are high on how it will meet the unmet demand. Compared to existing treatments that require daily administration, the new treatment is administered only 6 times a year, offering overwhelming convenience. With its accessibility barriers removed with reimbursement approval, the treatment is expected to gain influence quickly in the market. On the 17th of this month, GSK Korea held a meeting to commemorate the domestic launch of the Vocabria+Rekambys injection therapy and highlighted the treatment's effects and significance. The Vocabria+Rekambys combination was approved by the Ministry of Food and Drug Safety in February 2022 as a combination therapy for the treatment of HIV-1 infection in adult patients who are virologically suppressed, have no history of virological failure, and have no known or suspected resistance to cabotegravir or rilpivirine. Jae-Phil Choi, Professor of Infectious Diseases at Seoul Medical Center Jae-Phil Choi, Professor of Infectious Diseases at Seoul Medical Center, who presented at the event, stated, “Thanks to advancements in treatment that allow effective suppression of the virus, HIV has become a chronic condition that can be managed for life, similar to diabetes or hypertension. However, despite advancements in HIV treatment, social discrimination and stigma against people living with HIV remain widespread in South Korea.” According to Professor Choi, negative perceptions toward HIV influence treatment adherence among infected individuals, leading many to hesitate about seeking active early treatment and serving as a barrier to continuing treatment. According to the 2024 HIV Treatment Awareness Survey conducted by Love4One, a group representing people living with HIV, 73% of respondents in Korea reported feeling anxious that taking HIV medication might expose their status to others or attract unwanted attention. While conventional HIV treatments require daily oral dosing (365 days a year), injectable therapy using Cabotegravir (Vocabria) can reduce the dosing frequency to as little as once a month or once every two months—up to just 6 times a year. These advantages are expected to be effective in alleviating the anxiety caused by social stigma, which is one of the major challenges faced by HIV-infected individuals. Professor Choi emphasized, “Domestic HIV-infected individuals feel a significant psychological burden when taking medications, and as a result, they prefer long-acting HIV injections over oral medications that require daily intake. The Vocabria+Rekambys injection therapy could serve as an option that reduces anxiety about disclosure of infection status and alleviates the inconvenience and concerns associated with daily dosing, thereby providing high treatment adherence and satisfaction.” “High demand for bi-monthly dosing, sufficient flexibility in administration” Next, Professor Yeon-Sook Kim of the Department of Infectious Diseases at Chungnam National University Hospital, who participated in the clinical trial of the Vocabria+Rekambys injection therapy, stated that considering the treatment efficacy of the regimen, it may be possible to adjust treatment options according to the lifestyles of people living with HIV. Yeon-Sook Kim, Professor of Infectious Diseases at Chungnam National University HospitalProfessor Kim stated, “Analysis of data from HIV-infected individuals in Asia (n=41), including Korean HIV-infected individuals in the Phase IIIb clinical trial of the Vocabria+Rekambys injection therapy, showed that 83% of participants maintained viral suppression at Week 96 of treatment, with no reported cases of defined virological failure. This suggests that the Vocabria+Rekambys injection therapy could be an effective treatment option for HIV-infected individuals in Korea.” Professor Kim added, “A survey of HIV-infected individuals in Korea showed a high demand for ‘long-acting treatment with less frequent dosing’ for HIV treatment. With the recent reimbursement approval, it is worth considering changing the treatment option to a long-acting HIV injection according to the lifestyle of infected individuals.” However, along with expectations for reimbursement for the Vocabria+Rekambys injection therapy, there is also the concern that patients may feel burdened by having to visit the hospital more frequently. In the case of the Vocabria+Rekambys injection therapy, there is a 7-day period before and after the standard administration cycle, allowing for a total of 14 days of flexibility in administration, but this means that some patients may find it difficult to switch depending on their circumstances. “From the patient's perspective, there are cases where it is difficult to take time off work, and these patients receive prescriptions for oral medication once every 6 months. In such cases, it may be difficult to recommend switching to an injection therapy. However, for patients who typically receive a prescription every 3 months, we can consider switching to a long-acting injection administered every 2 months.” Professor Kim added, “Additionally, in cases where it is difficult to align the administration schedule due to overseas business trips, it is possible to reintroduce oral therapy. Since it is possible to switch back to oral medication after using the injection therapy, we believe there is sufficient flexibility in its administration.”
- Policy
- Petition filed urging expedited reimbursement of Livmarli
- by Lee, Jeong-Hwan Jun 17, 2025 06:00am
- A national petition has been filed to urge for the health insurance reimbursement of Livmarli (maralixibat), which is used to treat pruritus (itching) in patients with Alagille syndrome. The petition period runs until the 12th of next month, with over 1,600 signatures signed as of the 16th. Alagille syndrome is a condition in which the intrahepatic bile duct becomes significantly reduced in number (bile duct paucity), preventing bile from being excreted from the liver. This leads to its accumulation in the liver and is often accompanied by complications affecting the cardiovascular system, skeletal system, eyes, and skin. The drug is indicated for “biliary pruritus in patients with Alagille syndrome aged 1 year or older,” in Korea, and is imported by GC Biopharma. Livmarli is the first treatment in Korea for pruritus in patients with Alagille syndrome and is expected to be of great help to patients suffering from itching skin and other symptoms. According to data from the Health Insurance Review and Assessment Service, as of 2021, there are 136 patients with Alagille syndrome in South Korea. Livmarli obtained domestic marketing approval in February 2023, but it is not yet covered by health insurance. A petitioner who identified herself as Kim, a mother of a child with Alagille syndrome, wrote that her child is receiving treatment at Severance Hospital but is facing difficulties in treatment due to the lack of health insurance coverage for Livmarli. Kim explained that medical staff suggested participating in a clinical trial for another treatment, Bylvay Cap (odevixibat), but that this was not possible due to the child's young age. She added that there is a medical necessity to prioritize the use of novel drugs over liver transplantation for infants who have passed their first birthday and that the medical staff recommended Livmarli as an effective treatment option for such. This is why Kim launched a petition calling for the immediate reimbursement of Livmarli. Kim said, “The itching and skin damage (caused by Alagille syndrome) are destroying my child's daily life,” adding, “Xanthomas are not merely a cosmetic issue, but a serious indicator of how much bile and fat are accumulating in the body.” “For such a young child like mine, the opportunity and choice to alleviate symptoms with medication rather than undergoing a major surgery like a liver transplant is desperately needed. Rare diseases are not something families can face alone. It's heartbreaking that treatments exist but must be given up simply because they are not covered by insurance.”
- Opinion
- [Reporter’s View] Expectations for the second pilot project
- by Eo, Yun-Ho Jun 17, 2025 05:59am
- Several drugs that were undergoing concurrent regulatory approval and reimbursement evaluations for improved patient access are now approaching commercialization. However, whether these drugs will actually receive reimbursement coverage remains uncertain despite expedited approval timelines. Since 2023, the Ministry of Health and Welfare has been running a pilot program integrating the drug approval, reimbursement evaluation, and pricing negotiation processes specifically for drugs treating life-threatening conditions and rare or intractable diseases. The aim was to accelerate the timeline for new drug reimbursement under Korea’s National Health Insurance system. In October last year, the government selected the first two candidate drugs under the initial pilot program: ‘Qarziba’ (dinutuximab), a pediatric rare disease treatment, and ‘Bylvay. However, Bylvay failed to pass the Health Insurance Review & Assessment Service’s Drug Reimbursement Review Committee review. Even Qarziba, which was eventually listed for reimbursement, faced a temporary setback during the review process. Ten drugs applied for the second round of the pilot program in 2024, and three were selected: MSD Korea’s sotatercept (Winrevair) for pulmonary arterial hypertension, UCB Pharma Korea’s fenfluramine (Fintepla) for Dravet syndrome, and CuroCell’s anbal-cel (Rimqarto) for large B-cell lymphoma. All three are expected to be commercialized in Korea within this year. Eligibility criteria for the second round of the pilot program were as follows: ▲ drugs that can apply for both approval and reimbursement by June 2025, ▲ treatments for rare or life-threatening conditions with a life expectancy of less than one year with sufficient efficacy, ▲ drugs with no current alternatives or those that offer clinically significant improvements, and ▲ drugs designated or eligible for expedited approval under the GIFT program (Global Innovative Drug Fast Track) by the Ministry of Food and Drug Safety. The criteria clearly specify drugs urgently needed in clinical settings. While streamlining the reimbursement timeline for innovative drugs has long been discussed, and some procedural deadlines have indeed been shortened, doubts remain: Has the process truly become faster? Even for Qarziba, the first pilot drug, it took over one year for the drug’s reimbursment listing. The concurrent approval and pricing review system does not guarantee smooth or timely outcomes. In other words, transparency and speed remain key concerns for the system. New drugs must not be left in regulatory limbo – left to blindly await the government’s decision. As the second pilot program unfolds, this reporter hopes that the combined efforts of all parties will result in a clearer and shorter listing process.
- Company
- Lotte-Axcelead-Kanaph signs MOU for joint ADC development
- by Kim, Jin-Gu Jun 17, 2025 05:58am
- Lotte Biologics announced on the 16th that it has signed a three-party memorandum of understanding (MOU) with global new drug development company Axcelead and innovative new drug development company Kanaph Therapeutics to establish an ‘ADC Toolbox’ for the development of antibody-drug conjugates (ADC). Under the agreement, the three companies will collaborate on joint research and development of linkers and payload technologies, which are key for the development of antibody-drug conjugates, which are regarded as next-generation anticancer drugs. Axcelead is a global contract research organization (CRO) spun off from Takeda Pharmaceutical in Japan. It will utilize Takeda's library of over 1.2 million compounds and more than 1,000 new drug development data to identify novel payload candidates that have not been applied to existing ADCs. Kanaph Therapeutics will focus on building an innovative platform that overcomes the limitations of existing linkers and payloads in ADC development. The developed linkers, payloads, and other results will be transferred to Lotte Biologics, based on which the company will strengthen the competitiveness of its ADC platform, including SoluFlex Link. Through the collaboration, Lotte Biologics plans to provide an ADC toolbox service that allows customers to select and utilize various technologies according to their needs. This is expected to further strengthen its one-stop platform service, which covers everything from research and development to GMP production for ADC modalities. A Lotte Biologics representative said, “The agreement marks another step forward in establishing a differentiated ADC platform and toolbox. We will continue to strengthen our partnership with both companies to enhance our ADC competitiveness in the global market and provide patients with more innovative treatments.” An Axcelead representative said, “We are very pleased to be able to forge a strategic partnership for the development and advancement of ADC platform technology and services. Based on our proprietary new drug development platform, we will contribute to the development of innovative treatments.” A Kanaph Therapeutics representative added, “Through this collaboration, we will strive to build a diverse toolbox of linkers and payloads that can overcome the limitations of existing ADC drugs and accelerate the development of innovative new drugs.”
- Opinion
- [Reporter's View] GMP standards for sterile products
- by Lee, Hye-Kyung Jun 17, 2025 05:58am
- The Ministry of Food and Drug Safety (MFDS) is devising measures to reduce the burden on the pharmaceutical industry ahead of the implementation of the 'Revised PIC/S Good Manufacturing Practices (GMP) Guide for Sterile Medicinal Products (guidelines on manufacturing and quality control of medicines)' in December. Following the administrative announcement of revised guidelines in 2023, the MFDS has granted a two-year grace period. Therefore, the MFDS has planned a solution to lessen the burden, rather than an extended grace period as requested by several pharmaceutical companies. Strengthened GMP standards for sterile medicinal products include ▲systemic establishment·implementation of contaminant management methods for sterile medicinal products ▲establishment of separate GMP for cutting-edge technology biotechnology medicines ▲specifying detailed formulation and selection process·methods for products meeting GMP standards. Establishing contamination-control strategies is most important, but establishing a strategy for each lot number requires substantial manpower and investment. Approximately 100 companies in South Korea are reportedly manufacturing sterile products. In fact, since late last year, news of sterile production halts has been circulating, primarily among some manufacturers. For instance, Ildong Pharmaceutical's 'Ativan,' which had experienced years of supply halt and re-production, recently announced a final halt to both supply and production. According to the MFDS, this is due to the company's internal circumstances. It is also rumored that the decision to withdraw was made due to a combination of existing supply concerns, such as the cost-effectiveness of reinvesting in facilities, given the strengthened GMP standards. MFDS's consistent response when asked has been 'no further grace period.' Then, on the 11th, the MFDS Quality Management Division proactively requested a meeting with reporters. The MFDS explained that they had met with factory managers from approximately 20 manufacturers of sterile products last month. The reason they couldn't hold a press briefing immediately was their desire to jointly explain the ongoing 'Research on the GMP Guide for Sterile Products Implementation Plan' with the Korea Pharmaceutical and Bio-Pharma Manufacturers Association. MFDS has been conducting research jointly with the association since last year to alleviate the industry's burden related to the strengthened management of GMP for sterile products, aiming for standard relaxation. They are already in the mid-phase of research with three companies, HK inno.N, JW Pharmaceutical, and Daehan Pharmaceutical, which produce over 90% of large-volume intravenous fluids. If this research is successful, standards for large-volume intravenous fluids are expected to be relaxed first. From a quality perspective, they were preparing technical support measures to alleviate the industry's burden resulting from the actual implementation of the strengthened standard. However, a question arises here. While technical and regulatory support measures are being prepared to apply GMP standards at the same level as PIC/S member countries to domestic sterile product preparation manufacturers, has an alternative plan been prepared for cases where smaller companies, facing difficulties in facility and personnel investment despite this support, decide to abandon sterile product preparations? The disappointing part was the Quality Management Division's ambiguous response, suggesting that the Biopharmaceutical Management Support Team might handle supply-related issues rather than the Quality Management Division. It sounded like, 'GMP standards are our division's responsibility, but supply is another division's responsibility, so we don't know.' MFDS expresses concern that it might appear as if companies are abandoning the supply of sterile products, such as injectables, solely due to the strengthening of GMP standards. However, these two issues are inseparable. Many sterile product preparations are designated as shortage prevention drugs (SPD) or national essential medicines. This designation implies that the government intends to manage them because they are not profitable. Now, a situation has arisen where companies must invest anywhere from several billion to tens of billions of KRW in facilities and manpower for sterile product preparations that yield almost no profit. Consequently, it's inevitable that cases will emerge where companies decide to withdraw products after weighing investment costs against profitability. Therefore, instead of considering the issues of standards and supply separately, we hope that they will be addressed together, and solutions will be devised to reduce the burden on the pharmaceutical industry and alleviate public anxiety caused by supply instability.
- Company
- New RNAi drug 'Rivfloza' gets ODD in KOR
- by Eo, Yun-Ho Jun 16, 2025 06:04am
- The rare genetic disorder treatment 'Rivfloza' has been designated as an orphan drug in South Korea. The Ministry of Food and Drug Safety recently announced this on its notification board. Rivfloza (nedosiran) is indicated to treat children over 9 years of age and above and adults with 'primary hyperoxaluria type 1 (PH1)' and relatively preserved kidney function. Rivfloza was approved by the U.S. Food and Drug Administration (FDA) in October 2023. It is the first RNAi-based rug developed using Novo Nordisk's GalXC RNAi technology platform. The efficacy of Rivfloza was demonstrated through the results obtained from the Phase 2 PHYOXTM 2 study and the interim analysis data from the Phase 3 PHYOXTM 3 extension study. In the PHYOXTM 2 study, the Rivfloza-treated group showed a significantly lower 24-hour urinary oxalate (Uox) excretion rate at 90-180 days compared with the start of the administration. The study measured the changes in the 24-hour Uox excretion rate from the starting date using the area under the curve (AUC) analysis method. The results have shown that the average linear squares (LS) difference in 24-hour Uox excretion rate between the patient group treated with Rivfloza for 90 days and the control group was 4976. Furthermore, the interim results of the PHYOX3 extension study confirmed that reduced 24-h Uox excretion was maintained in 13 patients who received additional treatment of Rivfloza for 6 months. Meanwhile, PH1 is a rare genetic disorder causing oxalate overproduction in the liverm with an estimated prevalence of 1 in 38,600 people in the world. PH1 is the most common clinically out of three types of primary hyperoxaluria (approximately 80%). It is a metabolic disorder primarily affecting the kidney and may cause progression of kidney damage.
- Policy
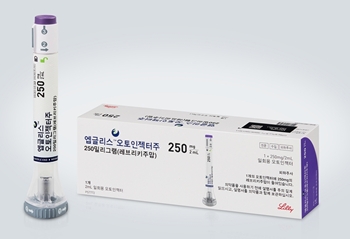
- Atopic dermatitis drug Ebglyss reimbursed from next month
- by Lee, Tak-Sun Jun 16, 2025 06:03am
- With pricing negotiations between the National Health Insurance Service and the manufacturer of the new atopic dermatitis drug ‘Ebglyss Autoinjector (Lebrikizumab, Lilly Korea)’ complete, the drug is expected to be listed for reimbursement next month in Korea. Once listed, the number of biological agents available for atopic dermatitis will increase from two—Dupixent (dupilumab) and Adtralza (tralokinumab)—to three. According to industry sources on the 13th, the NHIS recently updated its website with news of the agreement made on Ebglyss Autoinjector. In August 2024, the Ministry of Food and Drug Safety approved this drug as a treatment for the treatment of moderate-to-severe atopic dermatitis in adults and adolescents 12 years of age and older (weighing at least 40 kilograms) who are inadequately controlled by topical therapies or for whom such treatments are not recommended. In February, the drug’s reimbursement application was approved by the Drug Reimbursement Evaluation Committee of the Health Insurance Review and Assessment Service. At the time, the condition was attached that the adequacy of its reimbursement would be recognized if the company accepted the price below the initially assessed value. Lilly Korea accepted such a price and began negotiations with the National Health Insurance Service in March." It is highly likely that Ebglyss waived drug price negotiations as it accepted a price below the weighted average price of existing atopic dermatitis drugs covered by the national health insurance, and would only have negotiated the estimated claims amount with the NHIS. Ebglyss demonstrated its clinical efficacy and safety profile in a pivotal Phase III clinical trial and is expected to become a first-line treatment option for patients with atopic dermatitis in Korea. The clinical studies on which the approval was based on are the Phase III ADvocate-1, ADvocate-2 and ADhere trials. The trials evaluated the clinical efficacy and safety of Ebglyss in 1062 adults and adolescents with moderate-to-severe atopic dermatitis. In ADvocate-1 and ADvocate-2, which evaluated Ebglyss as a monotherapy, Ebglyss improved outcomes, with 58.8% and 52.1% (16.2% and 18.1%, respectively in the placebo arm) achieving Eczema Area and Severity Index (EASI) 75; and 38.3% and 30.7% (9% and 9.5%, respectively in the placebo arm) achieving EASI 90 during the induction period (weeks 0-16) compared to placebo. Also, after one year of maintenance therapy (Week 52), 81.7% of the Ebglyss arm achieved EASI 75 (vs. 66.4% in the placebo arm) and 66.4% achieved EASI 90 (vs. 41.9% in the placebo arm), demonstrating significant symptom improvement in the long term. The most commonly reported adverse events following treatment with Ebglyss were conjunctivitis (6.9%), injection site reactions (2.6%), allergic conjunctivitis (1.8%), and dry eye (1.4%), with the majority of adverse events being mild or moderate and not leading to treatment discontinuation. Recently, the government has applied reimbursement for cross-administration of biological agents and JAK inhibitors used to treat severe atopic dermatitis, and Ebglyss is expected to benefit from this as well. Patients are also expected to benefit from the increased biological agent options and lower drug prices.
- Policy
- Roche’s SMA drug Evrysdi Tab approved in Korea
- by Lee, Hye-Kyung Jun 16, 2025 06:03am
- The table formulation of Roche's blockbuster drug for spinal muscular atrophy (SMA), Evrysdi (risdiplam), has received marketing authorization in Korea. On the 13th, the Ministry of Food and Drug Safety approved Roche Korea's ‘Evrysdi 5 mg (risdiplam).’ With the approval, SMA patients in Korea may now be prescribed the 5 mg tablet formulation in addition to the existing liquid oral solution, enabling easier intake. Evrysdi is the first oral treatment for SMA and has the advantage of self-administering without location restrictions. In addition, the newly approved Evrysdi Tab is the first tablet formulation for SMA treatment. The 5mg tablets can be swallowed whole or dispersed in water and may be stored at room temperature. The existing liquid solution will continue to be available, and patients weighing 20 kg or more and aged 2 years or older are eligible to take the tablet formulation. Spinal Muscular Atrophy (SMA) is a systemic disorder caused by a deficiency of the Survival Motor Neuron (SMN) protein, which is essential for motor function. The disease affects not only neuromuscular systems but also respiratory muscles, cardiac rhythm, skeletal muscles, joints, and the autonomic nervous system. Evrysdi is a splicing modifier that binds to the immature pre-mRNA of the SMN2 gene, increasing and maintaining the levels of Survival Motor Neuron (SMN) protein throughout the patient's body. It can cross the blood-brain barrier, allowing for even distribution across the entire body, including the central nervous system. In February, the U.S. FDA approved Evrysdi based on the results of a bioequivalence study. In the trial, Evrysdi 5 mg Tab and the existing liquid formulation demonstrated equivalent absorption of the active ingredient risdiplam. Meanwhile, in Korea, Evrysdi Dry Syrup 0.75 mg/mL (risdiplam) was approved in 2020 and has been reimbursed since October 2023, three years later. Evrysdi is currently reimbursed for the treatment of 5q Spinal Muscular Atrophy in patients who received a genetic diagnosis of 5q SMN-1 deficiency or mutation that ▲ have 3 or fewer copies of SMN2 even before the onset of symptoms, and are less than 6 months old at the time of treatment initiation; or ▲ have SMA types 1-3 with clinical symptoms and signs related to SMA and are not on permanent ventilation.
- Company
- Anti-PD-1 immunotherapy 'Zynyz' gets ODD in KOR
- by Eo, Yun-Ho Jun 16, 2025 06:02am
- Product photo of Zynyz (retifanlimab) The checkpoint inhibitor immunotherapy 'Zynyz' has been designated as an orphan drug in South Korea. The Ministry of Food and Drug Safety (MFDS) has recently announced this through its notification board. It is indicated to treat relapsed or metastatic locally advanced Merkel cell carcinoma (MCC). Zynyz (retifanlimab) obtained U.S. approval in 2023 through the FDA's expedited approval program. MCC is associated with fast cancer cell growth and high metastatic rate, thus known for poor prognosis. Therefore, a first-line treatment option that can bring about a continuous response in metastatic MCC patients is necessary. The basis of accelerated approval of Zynyz is the Phase 2 PODIUM-201 study involving 65 patients with relapsed or metastatic locally advanced MCC who have not received prior systematic therapy. The study participants were treated with 500 mg Zynyz every 4 weeks for 24 weeks until they experienced progression of disease or non-tolerable toxicity level. The study's primary goal was set as the overall response rate (ORR) assessed by an independent review committee according to the RECIST guidelines (version 1.1). The secondary goals included the duration of response (DOR), disease control rate (DCR), progression-free survival (PFS), and overall survival (OS), and safety. The study results showed that the ORR of Zynyz was 52.2% (95% CI 40~65). In patients who showed responses, 18% of those had complete remission, and 34% had partial remission. The range of DOR was 1.1~24.9 months. 76% of the patients had DOR lasting over 6 months, and 62% had DOR lasting over 12 months. Meanwhile, Zynyz was recently approved by the FDA for additional indication to treat anal squamous cell carcinoma. It was the first immunotherapy to be approved. The basis of approval was the Phase 3 POD1UM-303 and the Phase 2 POD1UM-202 studies.