- LOGIN
- MemberShip
- 2025-12-21 23:06:47
- Company
- Zuellig Pharma's performance fluctuates after a brief reboun
- by Son, Hyung Min Apr 21, 2025 05:54am
- Zuellig Pharma Korea, a global pharmaceutical distributor that had experienced ups and downs in its external growth, successfully rebounded last year. Zuellig Pharma's sales declined for 4 consecutive years after recording sales of over KRW 1 trillion in 2020 but showed signs of recovery by taking on the domestic distribution of new drugs from multinational pharmaceutical companies. According to the Financial Supervisory Service on the 18th, Zuellig Pharma's sales last year were KRW 889.3 billion, up 4.8% from the previous year. Operating profit was KRW 4.3 billion, similar to the previous year. Zuellig Pharma is the Korean subsidiary of a Swiss global pharmaceutical distribution company that entered the Korean market in 1998. As the first global distributor to enter the Korean market, it faced strong opposition from the domestic industry. The Korea Pharmaceutical Distribution Association formed the Zuellig Countermeasures Committee and took strong measures to prevent Zuellig Pharma from monopolizing the supply of global pharmaceutical companies' products. Nevertheless, Zuellig Pharma's sales continued to grow until 2021. The company's sales grew steadily from KRW 706.9 billion in 2015 to KRW 889.4 billion in 2016, then to KRW 970.9 billion in 2017. Zuellig Pharma recorded KRW 1.184 trillion in 2019, becoming the third company to exceed KRW 1 trillion in sales after Geo-Yong and Baekje Pharmaceutical. The company maintained its status in the trillion-won club in 2020 with sales of KRW 1.0372 trillion, but sales fell to KRW 910 billion the following year. In 2022, sales amounted to KRW 885.3 billion, a 2.7% decrease from the previous year. In 2023, sales decreased by 4.1% year-on-year to 850 billion won. Zuellig Pharma was hit hard by changes in the drug distribution environment. Before, Zuellig Pharma had grown through exclusive deals with multinational pharmaceutical companies. In particular, domestic drug distributors had to sign wholesale contracts with Zuellig Pharma in order to distribute drugs from multinational pharmaceutical companies. However, major multinational pharmaceutical companies began to utilize the distribution networks of Korean pharmaceutical companies, forging co-promotion agreements with domestic companies, gradually reducing Zuellig Pharma's market share. In addition, domestic pharmaceutical distributors obtained distribution rights through direct contracts with multinational pharmaceutical companies, reducing Zuellig Pharma's main source of revenue. For example, Geo-Yong directly distributes UCB Korea’s allergy treatment Zyrtec, and psoriasis treatment Bimzelx. Geo-Yong is also selling over-the-counter (OTC) drugs from multinational pharmaceutical companies, such as the contraceptive Mercilon. Furthermore, major domestic companies have established new logistics systems such as 3PL and 4PL to enhance their competitiveness. Logistics systems are categorized into four types (1PL/2PL/3PL/4PL) based on their structure. 3PL refers to outsourcing logistics operations to external companies, while 4PL refers to customized services that not only outsource logistics but also provide consulting on suitable logistics systems and IT-related solutions. Larger companies have adopted integrated logistics strategy models, establishing their own logistics IT systems and strengthening order, receivables, and collection management functions. As a result, Zuellig Pharma now faces competition in the utilization of 3PL/4PL logistics systems as well. In particular, domestic companies have equipped themselves with cold chain systems and are distributing major biological products such as Dupixent, putting a brake on Zuellig Pharma's external growth. Operating profit rebounded, but competition intensified In addition to Zuellig Pharma, other global pharmaceutical distribution companies such as DKSH and DB Schenker Korea, as well as domestic firms like Pico Innovation and Bluemtec have established online platforms, intensifying market competition. However, Zuellig Pharma managed to rebound last year with its first sales increase in 4 years. In particular, operating profit has also improved recently. Zuellig Pharma posted operating losses every year from 2017 to 2021. However, in 2022, it returned to profit for the first time in about 7 years with KRW 900 million. In 2023 and last year, it recorded KRW 4.3 billion, showing growth. Zuellig Pharma succeeded in increasing its operating profit by improving its cost ratio along with a reduction in sales and administrative expenses and employee wages. Thanks to its improved performance, Zuellig Pharma emerged from total capital erosion, which had continued for 2 years since 2020. Total capital erosion refers to a state in which a company's deficit grows so large that its surplus runs out and even its paid-in capital is eroded, resulting in negative total capital. Zuellig Pharma was in a state of complete capital erosion in 2020 and 2021, with total capital of – KRW 1.5 billion and -KRW 14.5 billion, respectively. Zuellig Pharma plans to achieve growth in sales and operating profit through the distribution of innovative new drugs. Last year, Zuellig Pharma became responsible for the distribution of the obesity treatment drug Wegovy. Wegovy is a glucagon-like peptide (GLP-1) obesity treatment that recorded sales of over KRW 60 billion in the fourth quarter of last year alone. Zuellig Pharma successfully secured the distribution rights for Wegovy thanks to its experience in distributing the obesity treatment Saxenda. Zuellig Pharma will also be responsible for the domestic distribution of the immuno-oncology drug Libtayo. Libtayo (cemiplimab) is currently approved in South Korea as a first-line monotherapy for advanced non-small cell lung cancer and as a treatment for metastatic or locally advanced cutaneous squamous cell carcinoma (CSCC) and recurrent or metastatic cervical cancer. Last year, Zuellig Pharma also formed a partnership with European consumer healthcare company Karo Healthcare to target the Asian market and signed a domestic distribution agreement for the athlete's foot treatment Lamisil.
- Company
- Sanofi’s MenQuadfi to be launched soon in Korea
- by Whang, byung-woo Apr 21, 2025 05:54am
- Sanofi's next-generation meningococcal vaccine is set to launch just 1 year after receiving approval in Korea, signaling the start of intense market competition. Pic of MenQuadfi According to industry sources, Sanofi is preparing to launch its invasive meningococcal disease vaccine MenQuadfi in the third quarter of this year. MenQuadfi is a fully liquid vial quadrivalent meningococcal vaccine that prevents meningococcal serotypes A, C, W, and Y, and is approved for a single dose for individuals aged 2 to 55 years. When compared for immunogenicity with existing quadrivalent meningococcal vaccines, MenQuadfi demonstrated non-inferiority for all four serotypes. Unlike Sanofi's existing meningococcal vaccine, which utilized the diphtheria toxid protein, MenQuadfi utilizes the tetanus toxoid protein and has increased antigen amount. Currently available meningococcal vaccines include GSK Korea’s Menveo and Sanofi’s Menactra. Both vaccines are indicated for the prevention of invasive meningococcal disease caused by Neisseria meningitidis serogroups A, C, W135, and Y. With the launch of MenQuadfi, the competitive landscape is expected to shift from “Menveo vs. Menactra” to “Menveo vs. MenQuadfi.” Sanofi has decided to discontinue Menactra upon the launch of MenQuadfi, but the exact timing of supply discontinuation will be dependent on market inventory levels. A Sanofi representative stated, “We decided to launch MenQuadfi based on the high demand for Menactra in the global market and the expansion of its indications. As a result, we have decided to discontinue Menactra. We will do our utmost to ensure an uninterrupted supply of meningococcal vaccines in the Korean market by adjusting the launch schedule of MenQuadfi in accordance with the depletion of Menactra inventory.” One of the differences between Menactra and MenQuadfi is the age at which they can be administered. Menactra can be administered from 9 months of age, while MenQuadfi is currently available as a single dose for individuals aged 2 to 55 years. However, as the age range for MenQuadfi is being expanded, the vaccine is expected to naturally replace Menactra in the market. In particular, while Menactra contained 4ug of meningococcal serum antigen, MenQuadfi contains 10ug of all four antigens. Meningococcal vaccination costs, from left, GSK Menveo Sanofi Menactra (Data = HIRA Before MenQuadfi’s launch, GSK had already launched Bexsero, a meningococcal group B absorbed vaccine. Bexsero is a vaccine for preventing meningococcal group B infections and differs from the existing Menveo in its scope of prevention. In other words, GSK has introduced a new meningococcal vaccine with a different scope of prevention, while Sanofi has unveiled a next-generation vaccine with enhanced prevention effects. According to IQVIA data, Menveo's sales in 2023 were KRW 52 billion, while Menactra's sales were KRW 5 billion. Given the significant sales gap between the two products, both companies are expected to focus on increasing their market share with the launch of next-generation vaccines. However, meningococcal vaccines are not classified as essential vaccines and are classified as premium vaccines, so price accessibility is expected to be an important factor. According to the Health Insurance Review and Assessment Service's non-reimbursable medical expenses, Menveo costs an average of KRW 142,805, while Menactra costs an average of KRW 142,072.
- Company
- Roche Korea's 'Lunsumio' available at general hospitals
- by Eo, Yun-Ho Apr 21, 2025 05:54am
- Product photo of Lunsumio The first GIFT-designated drug 'Lunsumio' can now be prescribed in general hospitals. According to industry sources, Roche Korea's CD20xCD3 bi-specifc antibody 'Lunsumio (mosunetuzumab)' has passed the drug committee (DC) of Asan Medical Center in Seoul. Lunsumio is the first medicine to be designated as a 'Global Innovative products on Fast Track (GIFT)' and obtained approval from the Ministry of Food and Drug Safety (MFDS) in November 2023. This drug can be prescribed for adult patients with relapsed or refractory follicular lymphoma (FL) after two or more systemic therapies. However, Lunsumio remains a non-reimbursed drug. Roche has applied for the 'approval-assessment package system,' in addition to the GIFT designation, but discussions on reimbursement have yet to progress. FL is a type of non-Hodgkin Lymphoma (NHL) that occurs when cells in the lymph system turn malignant. Because the symptoms of the disease progress slowly, about 80% of the cases are identified at stage III or Stage IV after the disease progresses. The prognosis for patients who relapse is poor. Median progression-free survival (mPFS) is 10.6 years for patients who received first-line treatment; however, mPFS drops to two years with third-line treatments, representing about 20%. Lunsumio is the first-in-class CD20xCD3 bi-specific antibody involving T cells for relapsed or refractory FL. It simultaneously binds to a protein CD3 on the surface of T cells, which are types of white blood cells and immune cells, and protein CD20 of the malignant B cell surface, designed for T cells to target B cells. It is a readily applicable product that can be administered without waiting for manufacturing, and patients can be treated without hospitalization. The administration duration is fixed to eight cycles. During this period, when a patient does not reach complete remission, the drug administration can be extended to 17 cycles. Professor Won Seog Kim of Samsung Medical Center's Hematology and Oncology said, "FL is considered a good type of lymphoma with a life expectancy of 20 years, but as patients experience repeated relapses, the disease becomes aggressive, and the prognosis worsens. Therefore, an effective treatment regimen with expected remission was urgent for patients with FL who have relapsed two or more times."
- Company
- Hope for polycythemia vera, Besremi, makes reimb progress
- by Eo, Yun-Ho Apr 21, 2025 05:53am
- Industry attention is gathering on the insurance reimbursement progress for the polycythemia vera treatment, Besremi. According to industry sources, PharmaEssentia Korea's new drug for polycythemia vera, Besremi (ropeginterferon alfa-2b-njft), has been determined cost-effective by the Health Insurance Review and Assessment Service's Pharmacoeconomic Evaluation Subcommittee. Accordingly, the procedure will proceed depending on whether the company accepts the government's proposal. As Besremi will gain a unique status in the field when listed, the industry expects the company and the government to derive positive results. This is the second attempt for Besremi’s reimbursement listing in Korea. In March 2023, the drug underwent the reimbursement process for refractory or intolerant polycythemia vera but failed to pass the Cancer Disease Review Committee in July of the same year. At the time, the Cancer Disease Review Committee determined that there was insufficient evidence to judge the clinical utility of Besremi as a second-line treatment. In response, PharmaEssentia resubmitted its application for reimbursement in March after adding domestic clinical data on Besremi and supplementing the evidence on the drug’s efficacy as second-line therapy, and the application passed CDDC review in July of the same year. At that time, the Cancer Disease Review Committee established the reimbursement standards for Besremi as a treatment for patients with polycythemia vera without splenomegaly accompanied by symptoms in low-risk groups (limited to patients requiring cytoreductive therapy) and high-risk groups. Besremi is a next-generation interferon treatment that selectively removes JAK2 mutations that cause polycythemia vera. It was developed to improve the purity and tolerability of existing interferons so that it can be administered every two weeks for the first 1.5 years and every four weeks thereafter. It is currently recommended for the treatment of PV in the National Comprehensive Cancer Network (NCCN) and European Leukemia Network (ELN) guidelines, regardless of prior treatment history. Polycythemia vera is a rare blood disorder where a somatic cell mutation in the bone marrow abnormally activates bone marrow function and produces excessive red blood cells. According to HIRA data, about 5,000 patients are affected with PV in Korea, and hydroxyurea is mainly used for the majority of patients. However, as the current reimbursed drugs are not curative and there are no new alternatives for patients who fail hydroxyurea treatment, there remains a high unmet need for the disease.
- Policy
- Comb cancer therapy issue has been resolved
- by Whang, byung-woo Apr 21, 2025 05:53am
- Changes will be brought to the health system as a patient's existing co-payment amount will remain the same for ongoing chemotherapy when a reimbursed cancer drug combined with a newly developed, non-reimbursed new drug. Previously, insurance coverage for combination therapy comprising two drugs was unavailable, placing a financial burden on patients. The recent changes to this policy are viewed positively. However, as more combination therapies with new drug-new drug combinations are being approved, there are discussions about the need to establish procedures. The Ministry of Health and Welfare (MOHW) has recently issued an administrative notice proposing partial revision to the 'Detailed Criteria and Methods for Applying Reimbursement (Drugs),' which included details on combination cancer therapy. Previously, if a non‑reimbursed drug was added to a regimen already covered by reimbursement, even the previously reimbursed drugs would lose their coverage, increasing patients' out‑of‑pocket costs. After the announcement, patient organizations and academics have proposed suggestions. In response, the Health Insurance Review and Assessment Service (HIRA) convened a Cancer Drug Review Committee (CDRC) meeting in October 2024 to establish a review policy for determining the reimbursement status of major combination therapies. Under the revisions, adding a non‑reimbursed anticancer drug to an existing reimbursed regimen will not affect the co-payment rate for the reimbursed drugs. In detail, a new clause states, 'When combining a reimbursed chemotherapy regimen with another anticancer drug, the existing co-payment for the previously initiated chemotherapy shall continue to apply to that regimen.' A pharmaceutical industry employee remarked, "The combination anticancer therapy included in this notice are first-line treatments that account for a relatively small share of the National Health Insurance expenditure, so there have been calls for improvement," and added, "We were expecting changes after the April 30 CDRC meeting, but it's good news to see the draft notification issued so quickly. From a pharmaceutical company perspective, this change is truly significant." The partial revision notice announced by the MOHW exemplifies the case of AstraZeneca’s immuno‑oncology drug Imfinzi (durvalumab), which was under discussion for biliary tract cancer reimbursement last year. At that time, the CDRC maintained Imfinzi as non‑reimbursed for first‑line treatment of biliary tract cancer while recognizing reimbursement only for the other combination therapy drugs, gemcitabine and cisplatin chemotherapy (GemCis). New drug+new drug combination therapy gains attention, demands for improving the reimbursement process↑ As issues for combination therapy comprising an existing first‑line chemotherapy agent with a new drug are likely to be resolved, interest is growing in whether a reimbursement process for "new drug + new drug" combinations can be established. In fact, with more multinational companies having applied for reimbursement of combination therapies that include innovative anticancer agents, requests for a formalized process have continued. According to discussions at the March 'Policy forum on improving cancer patient access to combination therapies,' 54 anticancer combination therapies have been approved in South Korea over the past five years. Of these, 28 cases add a new drug to an existing therapy, and 26 are combinations of two new drugs. In other words, roughly half of the recently approved combination therapies involve two novel agents. There are suggestions for institutional policies to ensure that reimbursement can be reviewed quickly and rationally when a combination therapy includes drugs from different companies. The Korea Research-based Pharmaceutical Industry Association (KRPIA) has formed a working group to devise solutions. (From left) Product photos of MSD Korea The government acknowledges the need to improve the system…limitations exist to mandating private companies A closer look reveals the challenges. When two new drugs from different companies are used for combination therapy, each company's circumstances, such as volume‑based pricing or price-volume agreement, make simultaneous reimbursement applications difficult. Currently, there is no basis for the two companies to coordinate their reimbursement status. If only one company applies, proving cost‑effectiveness can be problematic, and the therapy may remain split between reimbursed and non‑reimbursed drugs, contrary to the system's intent to reduce patient burden. While the government acknowledges the need for reforms, it also recognizes that it cannot mandate private pharmaceutical companies to comply. At the forum, Hee‑Yeon Park of the MOHW explained, "When combining new drugs+new drugs, we need additional measures. We are reviewing various approaches for reimbursement mediation, but there are aspects we cannot mandate due to each company's circumstances." Several ideas have been proposed similar to official notifications regarding generic drug pricing application cases. According to pharmaceutical industry sources, generics that enter the market after a delay instead of immediately after the patent expiry file for drug pricing review, HIRA will notify the original manufacturer, allowing the company to decide its response strategy. There is also a proposal to have HIRA notify other manufacturers when one company applies for an anticancer combination therapy reimbursement. Because companies do not publicly disclose their reimbursement applications, having HIRA coordinate and guide the review could aid in setting the directions. Additionally, experts have suggested applying a more flexible ICER threshold for combination therapies, recognizing that such regimens typically involve longer treatment durations than monotherapies. Therefore, proven innovative combinations should warrant a relaxed ICER criterion. A KRPIA official commented, "Several companies have agreed on the need to establish a clear process for combination therapy. We are gathering exemplary cases from abroad and will propose recommendations once we agree on the necessary steps."
- Company
- Vocabria+Rekambys may be prescribed in general hospitals
- by Eo, Yun-Ho Apr 18, 2025 05:59am
- The long-acting HIV drug Vocabria+Rekambys combination therapy may now be prescribed in general hospitals in Korea. According to industry sources, GSK Korea’s Vocabria (cabotegravir) and Janssen Korea’s Rekambys (rilpivirine) combination passed the drug committees (DCs) of various medical institutions in Korea, including Korea University Anam Hospital, Konkuk University Medical Center, Kyungpook National University Hospital, and Chung-Ang University Hospital. The combination has been gradually expanding its prescription areas before and after the reimbursement listing this month (April). The upper insurance price ceiling for Vocabria 30mg is KRW 16,303 per tablet and KRW 991,882 per vial. The Vocabria+Rekambys combination was approved by the Ministry of Food and Drug Safety in February 2022 as a combination therapy for the treatment of HIV-1 infection in adult patients who are virologically suppressed, have no history of virological failure, and have no known or suspected resistance to cabotegravir or rilpivirine. The advantage of this combination therapy is undoubtedly its convenience in administration. While existing HIV treatments require patients to take a tablet formulation once a day, the two injectable drugs will reduce the frequency of administration to once a month or once every two months with intramuscular injections, increasing satisfaction and reducing the burden on patients. The two drugs were originally developed as oral medications and then were developed into injectable drugs. While this long-acting injectable drug cannot cure HIV infection, it is a treatment that targets white blood cells to help lower and maintain the level of the AIDS virus. Meanwhile, the efficacy and safety of the Vocabria+Rekambys combination therapy was demonstrated in clinical trials in groups that received the drug once every four weeks or once every eight weeks. The combination was approved in Europe in December 2020. In the clinical trial, the most frequently observed adverse reactions in the group that received the Vocabria+Rekambys combination were injection site reactions, headache, fever, nausea, fatigue, asthenia, and myalgia. In addition, the indication for combination therapy has been expanded to include adolescent patients in Europe.
- Policy
- CKD approved for Januvia+Jardiance+metformin combo
- by Lee, Hye-Kyung Apr 18, 2025 05:59am
- Chong Kun Dang, which launched a combination drug that combines the DPP-4 inhibitor 'Januvia (sitagliptin)' and the SGLT-2 inhibitor 'Jardiance (empagliflozin),' has received approval for a triple combination drug that adds metformin to the same combination just one week later. On the 16th, the Ministry of Food and Drug Safety approved three dosage forms of Emsiformin XR (empagliflozin, sitagliptin, metformin): 5/50/750 mg, 12.5/50/750 mg, and 25/100/1000 mg. Earlier, on the 7th, the first combination of Januvia and Jardiance in Korea, Empamax S Tab (empagliflozin, sitagliptin), in two dosages forms—10/100 mg and 25/100 mg—was approved. Previously, the industry was focused on developing two-drug combination products combining sitagliptin with the SGLT-2 inhibitor ‘Forxiga (dapagliflozin),’ with 116 products currently listed in the approved product list. However, with the expiration of the empagliflozin substance patent approaching on October 23, domestic companies are developing various two- and three-ingredient combination drugs using sitagliptin and empagliflozin. In addition to empagliflozin monotherapy, “Jardiance Duo” (empagliflozin+metformin) and “Esgliteo” (empagliflozin+linagliptin) are also subject to much interest by domestic companies. In particular, in the case of Jardiance Duo, Korean companies have been featuring a sustained-release formulation not available in the original product, leading to the emergence of various new diabetes treatments that offer new combinations and formulations. In the case of Chong Kun Dang, after securing all rights including domestic distribution and manufacturing rights for Januvia from MSD in 2023, the company has developed and obtained approval for a three-drug combination that adds metformin to the sitagliptin+empagliflozin combination. For empagliflozin, Chong Kun Dang successfully avoided patent infringement by modifying the salt crystalline form of empagliflozin to L-proline, an amino acid, creating “empagliflozin L-proline.” The newly approved three-drug diabetes combination, Emsiformin XR Tab, stands out for being approved as a sustained-release formulation, allowing once-daily administration instead of the twice-daily regimen required by the immediate-release formulations. Meanwhile, according to the MFDS's list of notified drugs, more than 12 items are currently in the application process for approval as a triple combination drug (sitagliptin+empagliflozin+metformin) in addition to Chong Kun Dang.
- Policy
- Original-generic collusion prevention law introduced
- by Lee, Jeong-Hwan Apr 18, 2025 05:59am
- A bill has been proposed in the National Assembly to prevent collusion between original drug manufacturers and generic drug manufacturers from maintaining the domestic sales status of original drugs through illegal means. On the 17th, Representative Young-Seok Seo (Gyeonggi Province, Bucheon City, National Assembly Health and Welfare Committee) proposed a partial amendment to the National Health Insurance Act to reduce the price ceiling set for medical expenses reimbursed for drugs related to collusion and unfair trade practices. The current law stipulates that when a generic drug with the same ingredients is released, the price of the original drug that was first registered must be reduced. As more generic drugs are released, the price of the original drug will fall further, which will reduce corporate sales but improve the financial health of the health insurance system and consumer welfare. However, if the original drug manufacturer and generic drug manufacturers engage in unfair collusion or unfair trade practices to refrain from manufacturing or supplying generic drugs, the original drug can retain its status. While the companies may continue to maintain sales based on the existing drug price, the health insurance budget deteriorates, and consumers lose the opportunity to benefit from lower drug prices. In particular, even if unfair collusion activities or unfair trade practices that disrupt market order are detected and subject to government sanctions, the original drug's status is not revoked, allowing the continued acquisition of unfair sales and profits, which has also been pointed out as an issue. Rep. Young-Seok Seo has introduced a bill to address these issues by allowing the reduction or suspension of the drug price reimbursement granted for drugs related to unfair collusion actions or unfair trade practices. The bill also includes provisions to prevent pharmaceutical companies not involved in problematic actions from suffering losses due to reductions in the original drug's insurance price ceiling when launching generic drugs. Rep Seo emphasized, “The revised bill aims to prevent companies that violate market order in the pharmaceutical market, which is critical to public health and safety, from reaping unfair profits through distorted market structures. We hope that the revised bill will reduce the practice of pharmaceutical companies disrupting market order, thereby worsening the health insurance budget and increasing the consumers’ burden of medication costs.”
- Company
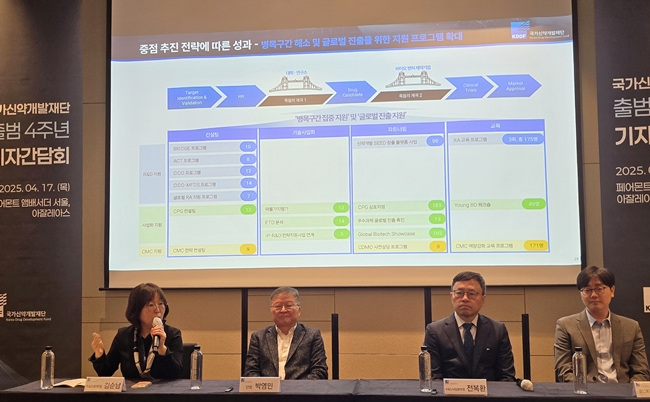
- KDDF "Continuity is important for support in new drug R&D"
- by Whang, byung-woo Apr 18, 2025 05:57am
- The Korea Drug Development Fund (KDDF), celebrated fourth year since launch, has emphasized its role as a 'supporter' rather than a 'management' in advancing successful new drug development. As it enters its fifth year and reaches a midpoint of the project duration, KDDF has emphasized the need for continuity and a centralized control tower. KDDF Ceo Park Yeong-min On April 17, KDDF Ceo Park Yeong-min held a press briefing to share the KDDF's achievements and future strategies on its fourth anniversary. KDDF program supports the entire drug development lifecycle, including candidate discovery, preclinical studies through Phase 1 and 2 clinical trials, and commercialization. It is a multi‑ministerial R&D initiative with KRW 2.1758 trillion (KRW 1.4747 trillion in government funding and KRW 701.1 billion in private investment) allocated over ten years through 2030. Since its 2021 launch, KDDF has supported 423 pipeline projects and plans to add 128 new projects this year, bringing its total to approximately 550. Ultimately, KDDF aims to strengthen the R&D ecosystem by improving the success rate of early‑stage technologies progressing to later development stages and building biotech venture capabilities. Furthermore, KDDF assists with global partnering and investment attraction to generate practical outcomes such as blockbuster new‑drug approvals and global technology transfers. As it reaches the midpoint of its ten‑year plan, KDDF will focus on enhancing its commercialization support this year alongside ongoing target and modality projects. To achieve these goals, KDDF has increased clinical project funding by 30%, raising support to KRW 4.55 billion for Phase 1 trials and around KRW 9.1 billion for Phase 2 trials. Previously, KDDF capped support at KRW 2 billion for non-clinical stages, KRW 3.5 billion for Phase 1, and KRW 7 billion for Phase 2. Park stated, "We aim to discover globally competitive molecules and will focus on new targets and modalities," and added, "By optimizing our commercialization support, KDDF can pioneer a new R&D model." "We will expand programs to resolve drug‑development bottlenecks and strengthen global competitiveness. KDDF will not merely provide support, but we will establish an efficient R&D structure." During the meeting, KDDF stressed that as a sunsetting program, it requires guaranteed continuity given the long timelines inherent in new‑drug development. Park said, "KDDF is a sunsetting program that must undergo a feasibility reassessment after ten years, which can create inefficiencies in later stages," and added, "Since the government has designated the bio‑pharma industry as a future growth engine, the organization supporting frontline drug development must operate without interruption." KDDF succeeded the previous multi‑ministerial new drug development program, which ran from 2011 until its closure in September 2020, and KDDF then launched in 2021. However, there was a roughly six‑month gap between the predecessor program's end and KDDF's launch, during which small biotech firms reportedly faced support disruptions that delayed their R&D for over six months. Given KDDF's fixed ten‑year timeframe, experts have called for follow‑up measures to ensure domestic drug developers do not abandon projects due to support gaps. Park said, "We need to double the budget for drug development to support more companies. New policy measures, such as supporting potential K‑Big Pharma, are needed so that KDDF could serve as the control tower for Korea's pharmaceutical and biotech industry."
- Policy
- Co-payments retained for non-reimb drug+reimb drug comb
- by Lee, Jeong-Hwan Apr 18, 2025 05:57am
- The Ministry of Health and Welfare (MOHW) has decided that, even if an additional or combination anticancer drug is added to a chemotherapy regimen already covered by health insurance, the initial chemotherapy will continue to be subject to the patient’s existing co-payment. Boehringer Ingelheim’s idiopathic pulmonary fibrosis and fibrosing interstitial lung disease treatment Ofev (nintedanib) will have new reimbursement criteria established, while the reimbursement standards for donepezil oral tablets and patches, such as Aricept tablets and Donerion patches, will be revised. The reimbursement criteria for rituximab injections (such as MabThera), ceftazidime (such as vancomycin), and ganciclovir injections (such as Cytovene IV) will also be updated. On April 17, the MOHW issued an administrative notice proposing partial revisions to the 'Detailed Criteria and Methods for Applying Reimbursement (Drugs).' The revision is aimed to take effect on May 1, and a public comment submission will run through April 21. Previously, if a non‑reimbursed drug was added to a regimen already covered by reimbursement, even the previously reimbursed drugs would lose their coverage, increasing patients' out‑of‑pocket costs. Under the revisions, adding a non‑reimbursed anticancer drug to an already reimbursed regimen will not change the co-payment rate for the reimbursed drugs. In detail, a new clause states, 'When combining a reimbursed chemotherapy regimen with another anticancer drug, the existing co-payment for the previously initiated chemotherapy shall continue to apply to that regimen.' The MFDS approved Ofev's new reimbursement coverage for chronic fibrosing interstitial lung disease among the indications. The coverage will be provided to patients with chronic fibrosing interstitial lung disease confirmed by high‑resolution chest CT (HRCT), excluding idiopathic pulmonary fibrosis. The reimbursement criteria include cases where ▲predicted forced vital capacity (FVC) ≥ 45% ▲ predicted diffusing capacity for carbon monoxide (DLco) ≥ 30% and < 80% ▲despite prior treatment (steroids, immunosuppressants), within the past 24 months one of the following: a relative decline in predicted FVC ≥ 10%; a relative decline of greater than 5% or less than 10% with worsening respiratory symptoms; or a relative decline of greater than 5% or less than 10% with HRCT documented fibrosis progression. Patients must be re‑evaluated every 12 months after treatment initiation (HRCT and pulmonary function tests), and if disease progression is confirmed (predicted FVC decline ≥ 10% within 12 months with HRCT worsening), administration must be discontinued. The reimbursement criteria for donepezil formulations state the dosage and duration for 3 mg oral tablets. The reimbursement criteria for 3 mg tablets indicate that ▲an initial dose of 3 mg once daily may be started to reduce adverse gastrointestinal reactions if needed, but use should not exceed 1–2 weeks ▲in underweight women (BMI < 18.5 kg/m²) aged ≥ 85 years who require ongoing 3 mg once‑daily dosing, reassessment should determine continuation based on evaluation methods. Moreover, if dosing at 3 mg once daily must continue beyond 6–8 weeks, a dosing justification form must be submitted. Reimbursement criteria for rituximab injections have been expanded to include myasthenia gravis. Eligible patients are those who are MuSK antibody–positive because they are refractory to at least one prior therapy (corticosteroids, azathioprine, cyclosporine, mycophenolate mofetil, tacrolimus, etc.) or unable to receive such therapies due to ▲serious adverse effects, and who have either moderate to severe myasthenia gravis (MGFA class IIa or higher) or ▲at least two myasthenic crises within the past year. Reimbursement is covered for rituximab at 375 mg/m² weekly for four doses or 1 g every two weeks for two doses, with retreatment permitted upon relapse. For vancomycin and ceftazidime, reimbursement has been expanded beyond their approved indications to include adult bacterial endophthalmitis. Vancomycin is reimbursed for intravitreal injection of 1 mg/0.1 mL administered at intervals of 3 days or more based on clinical findings (inflammation and infection control), and ceftazidime is reimbursed for intravitreal injection of 2 mg/0.1 mL or 2.25 mg/0.1 mL at intervals of 2 days or more. If combination use is clinically required, each drug's reimbursement criteria apply. For ganciclovir, reimbursement criteria have been added for acute retinal necrosis syndrome (ARN) and CMV retinitis (CMVR), expanding the reimbursement scope. Eligible patients are those ▲who are nonresponsive or intolerant to systemic antiviral therapy or ▲who have rapidly progressive, vision‑threatening retinal lesions; dosage is 2 mg/0.1 mL intravitreally once to three times weekly, with dose reductions permitted based on patient status.