- LOGIN
- MemberShip
- 2025-12-22 09:16:51
- Company
- Will Roche’s lymphoma drug Columvi be discussed for reimb?
- by Eo, Yun-Ho Oct 28, 2024 05:53am
- Will Columvi, the first bispecific antibody treatment option for lymphoma, enter the first step to its reimbursement within the year? Roche Korea’s CD20-CD3 bispecific antibody for diffuse large B-cell lymphoma (DLBCL), Columvi (glofitamab), may likely be redeliberated by the Health Insurance Review and Assessment Service's Cancer Disease Deliberation Committee meeting set to be held in November. Originally, there were hopes for its discussions in October, supported by strong requests from patient groups. The agenda was reviewed by CDDC in July but failed to set reimbursement standards at the time. Therefore, industry eyes are on whether Columvi can break through the barrier this time. Columvi was approved in Korea last December for the treatment of adult patients with relapsed or refractory diffuse large B cell lymphoma (DLBCL), after two or more lines of systemic therapy. The drug is a third-line treatment option for DLBCL, like Novartis’s chimeric antigen receptor (CAR)-T-cell therapy Kymriah (tisagenlecleucel). The two drugs have different benefits; therefore the choice will likely be based on each patient's condition and circumstance. Columvi demonstrated efficacy in the Phase I/II NP30179 trial in 155 patients with relapsed or refractory DLBCL after two or more prior systemic therapies. Results showed that Columvi achieved a complete response (CR) of 40% and an overall response rate(ORR) of 52%. The efficacy was also consistent across all subgroups. The most common adverse event was cytokine release syndrome (CRS). Adding to the encouraging data presented at the 2024 Congress of the European Hematology Association (EHA 2024), the company unveiled the results of the Phase III STARGLO study, which demonstrated an improvement in overall survival (OS) with Columvi. The STARGLO study enrolled patients with relapsed or refractory (R/R) diffuse DLBCL who were not eligible to receive an autologous stem cell transplant after one or more prior systemic therapies, or who had received two or more prior systemic therapies. In the primary analysis (median follow-up 11.3 months), Columvi and gemcitabine+oxaliplatin (GemOx) combination significantly improved the primary endpoint of OS with a 41% lower risk of death compared to rituximab+GemOx. Meanwhile, the Korea Leukemia Patients Organization had continuously requested the CDDC review for Columvi review in October and has also requested that Roche, the manufacturer, provide a financial sharing plan to expedite its reimbursement listing.
- Company
- "We have clinically proven Stelara for Koreans"
- by Moon, sung-ho Oct 28, 2024 05:53am
- Due to its wide variety of conditions, Crohn's disease requires customized long-term treatment depending on the disease type and inflammatory region. When treating patients with Crohn's disease, the location of the disease is challenging because the intestinal tract of the ileum (lower part of the small intestine) is narrow. Recently, the research results of the K-STAR study, the Real-World Evidence (RWE) study of Stelara, a drug containing the original ingredient ustekinumab, was conducted for the first time in Korean patients, were published in 'IBD (Inflammatory Bowel Diseases) Journal.' The K-STAR study followed the effects and safety of Stelara in Korean patients with Crohn's disease over a year. Discussion with Dr. Byong Duk Ye and Dr. Chang Kyun Lee who have presented the first RWE study conducted in South Korea.This research confirmed clinically and endoscopically improved effects and drug tolerance profile regardless of the disease-affected regions or disease type.다. On October 14th, Daily Pharm met with the research authors, Dr. Byong Duk Ye, a Professor at Asan Medical Center (Gastroenterology), and Dr. Chang Kyun Lee, a Professor at Kyunghee University (Gastroenterology), and heard about potential changes to the treatment strategy for Crohn's disease after the K-STAR research. ▶ We have heard that the study is the first study to use the Real-World Data collected from Korean patients with Crohn's disease. Ye: The K-STAR study is a RWE study conducted from April 2018 to April 2022. It enrolled 464 patients with Crohn's disease who have started the Stelara treatment in 44 medical centers. The study evaluated the results of all adverse reactions and the efficacy over the year after the Stelara treatment. The study was significant because it was the first Stelara RWE to involve Korean patients with Crohn's disease and a multi-agency Post-Marketing Survey (PMS) study where clinical response rate·remission rate, endoscopic remission rate, and improvements to biomarker index were comprehensively evaluated. Furthermore, 60% of the patients enrolled in the study already had complications, including stenosis and fistulas. After the Stelara treatment, these patients had no further advancement in Crohn's disease and remained stable for up to 1 year. Lee: The study is meaningful because it is an RWE that shows the distribution of disease types and conditions among Koreans undergoing treatments. Unlike previously presented real-world data (RWD)-based studies were retrospective, the K-START study is significant because it collected data over a year, following pre-planned criteria from the beginning of the study. ▶ Stelara monotherapy's clinical remission rate was similar to that of the concomitant use of the drug with immune modulators. What does it entail? Ye: Patients using immune modulators often report pain during treatment due to a variety of side effects. Because of this, using the drugs in combination was uneasy. The current research showed that the clinical remission rate of Stelara monotherapy was not significantly different from that of using Stelara in combination with the immune modulator. It lowered the occurrence of side effects due to the immune modulators and provided a medical cost-saving effect ▶ We would like to hear about the report on differences in the treatment outcomes of patients previously treated with a biological agent or not. Ye: In the research, higher treatment effects were observed in patients with no prior experience with a biological agent than patients with experience of such experience. At 16-20 weeks of treatment, combined effectiveness was 50.3% for patients with no prior experience with a biological agent and 30.7% for patients with prior experience. At 52-66 weeks of treatment, 47.7% and 36.0% of combined effectiveness were observed, respectively. Both follow-up periods showed significant differences. Based on these results, greater effects can be expected when Stelara, a biological agent, is used as the first-line treatment. In my opinion, the study's importance lies in having Korean patients with Crohn's disease as study participants and in using Stelara monotherapy as the first-line treatment of a biological agent without using the drug in combination with an immune modulator. Lee: Many patients registered to the previous RWD-based studies already have prior experiences with medication, so they have undergone drug switching. This study is particularly significant because the percentages of patients with prior biological agent treatment (53.4%) and without one (46.6%) are nearly similar. ▶ In the K-STAR study, what treatment effects of Stelara were observed in the regions affected by the disease? Ye: In this research, the clinical response rate was higher in patients with the disease affecting the ileum (L1) than in patients who have the disease spread to the colon (L2) or ileocolon (L3). Typically, Anti-Tumor Necrosis Factor (TNF) agents, which show strong anti-inflammatory effects, were considered for patients with terminal ileal Crohn's disease. However, this research demonstrated that Stelara could effectively treat terminal ileal Crohn's disease. ▶How would you think the Stelara-treatable patient group would change following this research? Lee: In Korean patients with Crohn's disease, the ileum is the most affected region. Through this research, Stelara was found to effectively treat terminal ileal Crohn's disease, and the treatable patient group has expanded. We could expect to achieve treatment effects when providing Stelaral monotherapy at an early stage in patients aged 65 years and older with terminal ileal Crohn's disease who were hesitant about undergoing immune modulators. Also, Stelara was proven effective in treating patients who initially attempted anti-TNF agents and then experienced diminishing effects. We can now consider various treatment methods in the clinical setting. Ye: Regardless of disease type, over 50% of all patient groups reached clinical response, clinical remission, and clinical remission without steroids when treated with Stelara. In other words, patients with Crohn's disease with accompanying complications who were not subject to surgeries had anti-TNF agents as a treatment option. Now, Stelara can be considered depending on clinical conditions. ▶Recently, drug prescription sequence is often discussed when treating IBD, such as Croh's disease. We are curious what drugs are primarily prescribed in treating Crohn's disease. Ye: Patient-customized prescriptions are important when prescribing drugs. Safety is foremost considered when prescribing to patients who are likely to have a high risk of side effects. Administration methods are important depending on patient lifestyles. We primarily consider treatment effects for patients with poor prognosis and need to modulate inflammation quickly. Lee: Drug prescription sequence differ depending on patient profiles, so nothing is absolute. Drugs with high safety profiles are primarily used in patients who are prone to having drug-associated side effects, and drugs with superior effects are used for patients who need to treat the inflammation quickly on top of safety. Additionally, the drug prescription order is selected after a comprehensive assessment of cost issues, insurance policies, and lifestyles. In conclusion, we think that the goal of the sequence is to aim for the long-term maintenance of the treatment by considering such treatment decisions.
- Company
- Januvia generics occupy 17% of market in 1yr
- by Kim, Jin-Gu Oct 28, 2024 05:53am
- Generic versions of the DPP-4 inhibitor diabetes drug ‘Januvia (sitagliptin)’ have expanded their share to 17% within a year of its launch. In the pharmaceutical industry, the assessment is that their penetration rate is somewhat slower compared to other DPP-4 inhibitor generics. In fact, the generic versions of Galvus (vildagliptin) and Tenelia (teneligliptin), which went off-patent before Januvia, gained market share similar to their original versions within a year of generic launch. Q3Prescriptions of Januvia and Janumet generics in Q3 reach KRW 5.1 billion…market share rate 17% According to the market research institution UBIST on the 28th, the outpatient prescription volume of sitagliptin monotherapy and sitagliptin-metformin combination therapy was KRW 30.2 billion in Q3 this year. This is down 13% from the KRW 34.8 billion in Q3 last year. In the sitagliptin monotherapy market, the generic products generated a combined prescription amount of KRW 1.6 billion. The original product, Januvia, generated KRW 5.8 billion during the period. The generic versions accounted for 22% of the single-drug market. In the sitagliptin-metformin combination market, the generics generated a combined prescription volume of KRW 3.5 billion. In the same period, the original Janumet-Janumet XR generated KRW 19.3 billion. The share of the generics in the combination market is around 15%. The generics of the entire Januvia series generated a combined prescription volume of KRW 5.1 billion. The prescriptions of the Januvia series generics have increased from KRW 2 billion in Q4 last year, KRW 3.6 billion in Q1 this year, KRW 4.5 billion in Q2, and KRW 5.1 billion in Q3. During this period, the share of generics expanded from 7% to 12% to 15% to 17%, etc. Quarterly prescriptions of Januvia, Janumet and their respective generics (Unit: KRW 100 million, Data: IQVIA) By company, Hanmi Pharmaceutical recorded the highest cumulative prescription sales of KRW 2.4 billion over the past year. Its single-agent drug ‘Sita Tab’ accounted for KRW 600 million and the combination drug ‘Sita Met XR’ accounted for KRW 1.9 billion. This was followed by Seoul Pharmaceuticals, Kyungbo Pharmaceutical, and Daewon Pharm with cumulative prescription sales of KRW 1.5 billion each. The rest of the companies have earned less than KRW 800 million in cumulative prescriptions over the past year. The 21 generic companies have accumulated less than KRW 100 million in cumulative prescriptions over the past year, which renders the average prescription revenue per company to less than KRW 100 million. Compared to Tenelia and Galvus...the speed of market penetration↓ The industry consensus is that the Januvia generics have not met expectations in terms of market penetration. Januvia's patent expired in September last year. Many companies were interested in the patent expiry of the product, as it had been the leading product in the prescription market for DPP-4 inhibitors worth KRW 600 billion a year. A total of 89 companies received approval for their generic versions, 52 of which launched products. Despite the rush to enter the market, the initial performance of the products has been disappointing. In fact, compared to other products in the same class, such as Tenelia and Galvus, Januvia generics have been slower in gaining market share. In the case of Tenelia-Tenelia M, the generic surpassed the original’s market share with a 51% share in its first year. Tenelia's patent expired in October 2022. Thirty-eight pharmaceutical companies launched generics simultaneously. Since then, Tenelia generics have quickly penetrated the market. In the first year of its launch, the combined generic prescription volume was KRW 13.1 billion, higher than that of the original's KRW 12.4 billion. In the case of Galvus-Galvus Met, the generic’s share reached 44% in the first year. The patent for Galvus expired in March 2022. Since then, generic products have steadily increased prescriptions. In the first year, combined generic prescriptions amounted to KRW 5.7 billion, significantly narrowing the gap with the original (KRW 7.4 billion). One of the reasons why Januvia generics struggled to penetrate the market earlier in its launch is that the market for DPP-4 inhibitor class diabetes drugs is already saturated. In addition to the Januvia series, the market is also dominated by originator products such as Zemiglo, Trajenta, Tenelia, Suganon, Galvus, Onglyza, Nesina, and Guardlet. Of these, Tenelia, Galvus, and Trjenta generics have emerged after their patents expired. Moreover, in the DPP-4 inhibitor diabetes market, overall prescription sales have been declining since the introduction of SGLT-2 inhibitors such as Forxiga and Jardiance. In this context, the entry of large numbers of Januvia and Janumet generics into the market, as well as the fierce competition, led to performance below expectations. This, coupled with supply and demand uncertainties during the initial launch of the generics, would have had a significant impact. Generic companies struggled to secure volumes for a while after Januvia's patent expired, as manufacturers of sitagliptin raw materials were unable to keep up with the sudden increase in demand from domestic pharmaceutical companies, leading to supply instability for Contract Development and Manufacturing Organizations.
- Company
- Will the ATTR-CM drug 'Vyndamax' receive reimb approval?
- by Eo, Yun-Ho Oct 25, 2024 05:49am
- Product photo of Vyndamax Cap. Will 'Vyndamax,' a new drug used to treat transthyretin amyloid cardiomyopathy, successfully be listed for insurance reimbursement? Pfizer Korea's Vyndamax (tafamidis 61 mg), a treatment for ATTR-CM (ATTR amyloidosis with cardiomyopathy), has recently passed the Drug Reimbursement Evaluation Committee (DREC) of the Health Insurance Review and Assessment Service (HIRA). It is an accomplishment after 2 years and 10 months after applying for reimbursement in 2021. The last hurdle is the drug price negotiations with the HIRA. At its first attempt at reimbursement in early 2021, Vyndamax failed to receive designation as an essential medicine. After that, the economic evaluation was conducted in the first half of the same year and a second attempt was made through the Risk Sharing Agreement (RSA) program. In April 2022, the drug had not passed the reimbursement criteria committee of the HIRA. It passed the committee review in July of the same year. However, after 9 months, it received a non-reimbursement decision from the DREC review. This time, it finally passed the DREC review. As a result, the industry's attention is on whether Vyndamax would pass the drug price negotiations and get the final listing. Meanwhile, Vyndamax is the only treatment option for ATTR-CM. ATTR-CM is fatal, where the overall survival is merely 2-3.5 years when not treated timely, but patients are often misdiagnosed as heart failures. The disease is known as having poor treatment outcomes due to inadequate treatment availability. Amid these difficulties, the efficacy of Vyndamax was demonstrated through the Phase ATTR-ACT study, which showed Vyndamax reduced the occurrence of cardiovascular-related events and improved 6 minutes walking test in CM patients. As a result, Korean doctors are claiming for the necessity of Vyndamax prescription. "Vyndamax can help patients by increasing the survival rate. As Vyndamax was approved in South Korea last year, it brought immense development in the treatment setting. However, it is not yet covered with insurance reimbursement, so patients cannot start treatment after getting diagnosed," Dr. Jung-Woo Son, a Professor of Wonju Severance Christian Hospital's Cardiology.
- Company
- K-new drugs Rosuzet·K-CAB dominate the prescription market
- by Chon, Seung-Hyun Oct 25, 2024 05:48am
- Pharmaceuticals developed by Korean pharmaceutical companies using their R&D capacities have strengthened their influence on the outpatient prescription market. Quarterly prescription sales of Hanmi Pharmaceutical's new combination drug, Rosuzet, and HK inno.N's K-CAB exceeded KRW 50 billion, ranking at the top. Astra Zeneca's anticancer agent, Tagrisso, also exhibits a high growth rate with its expanded reimbursement. According to drug market research company IQVIA on October 23rd, Rosuzet, a combination therapy used to treat hyperlipidemia, recorded the highest outpatient prescription amount by generating KRW 53.5 billion. Rosuzet exhibited growth of 17.5% compared to Q3 last year, leading the market for the past three quarters. Pharmaceuticals ranking by quarterly outpatient sales. Hanmi Pharmaceutical Launched in late 2015, Rosuzet is a combination drug for the treatment of hyperlipidemia. It is comprised of two active ingredients: Rosuvastatin and Ezetimibe. Since Rosuvastatin·Ezetimibe combination drugs are effective in lowering low-density lipoprotein-cholesterol (LDL-C) and cost less than taking two separate drugs, they are popular in the prescription market. From generating KRW 26.7 billion in prescription sales in Q3 of 2020, Rosuzet continued to exhibit a high growth rate, doubling in size over 4 years. In Q1, Rosuzet became first pharmaceuticals developed in South Korea to rank No.1, and it continued to maintain the top-rank for three consecutive quarters. Rosuzet's cumulative prescription sales for Q3 were KRW 153.6 billion, up 17.3 % year-over-year (YoY). It is likely to exceed KRW 200 billion in prescription sales. Rosuzet has exceeded KRW 100 billion in prescription sales for five consecutive years since 2020. K-CAB's prescription sales for Q3 amounted to KRW 50.4 billion, up 27.5% YoY, ranking No.2. It surpassed Lipitor in Q2 and became second. In Q3, it chased Rosuzet by a difference of KRW 3.2 billion, placing among top-ranked pharmaceuticals. K-Cab's cumulative prescription sales for Q3 were KRW 142.2 billion, up 24.6% from the previous year. K-CAB, approved as the 30th new drug developed in South Korea in 2018, is an antiulcer drug of the 'Potassium-Competitive Acid Blockers (P-CAB)' class. It blocks gastric acid by competitive binding of proton pumps and potassium ions, which are expressed in the gastric parietal cells catalyzing gastric acid secretion in the final step. K-CAB quickly shows drug effects faster than the conventional proton pump inhibitors (PPI). It continues to exhibit a high growth trend with its benefit of taking the medication regardless of food intake. K-CAB secured five indications serially, including treatment of erosive gastroesophageal reflux disease, treatment of non-erosive gastroesophageal reflux disease, treatment of gastric ulcer, antibiotic combination therapy for the eradication of Helicobacter pylori in patients with peptic ulcer or chronic atrophic gastritis. K-CAB's sales partner changed from Chong Kun Dang to Boryung this year, but the company continued to show high growth. HK inno.N and Boryung signed a co-promotion agreement at the end of last year, and they have started to co-sell K-CAB and the Kanarb family products. Astra Zeneca's anticancer agent, Tagrisso, also exhibited significant growth. In Q3, Tagrisso generated KRW 36.5 billion in outpatient prescription sales, up 59.4% YoY. It skyrocketed 72.4% in two years from KRW 21.2 billion in Q3 of 2022. Tagrisso is an epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor (TKI). EGFR-TKI is a targeted anticancer agent prescribed to patients with metastatic non-small cell lung cancer (NSCLC) who have accompanying EGFR mutations. Starting this year, Tagrisso expanded the National Health Insurance reimbursement scope to include the 'first-line treatment of locally advanced or metastatic non-small cell lung cancer (NSCLC) with specific genetic mutations' along with Yuhan's Leclaza. In Q4 of last year, Tagrisso recorded KRW 21 billion in outpatient prescription sales, showing a 73.6% increase over three quarters due to expanded reimbursement. Anticancer agents are primarily prescribed for inpatients. However, Tagrisso significantly increased outpatient prescription sales due to its oral formulation. Expanded during a similar period as Tagrisso, Leclaza recorded KRW 12.8 billion in outpatient prescription sales for Q3, up 86.1% from last year. Daewoong Bio's Gliatamin, a brain function-improving drug containing choline alfoscerate, recorded KRW 41.2 billion in Q3 prescription sales, down 4.4% from the previous year. It ranked fourth overall. Despite several issues related to its efficacy, reduced reimbursement scope, and retrieval negotiation order, it continued to influence the market for prescription drugs. In Q3, Chong Kung Dang's choline alfoscerate containing Chongkundang Gliatirin recorded KRW 31.1 billion, a 10.9% increase from the previous year, placing among the top.
- Company
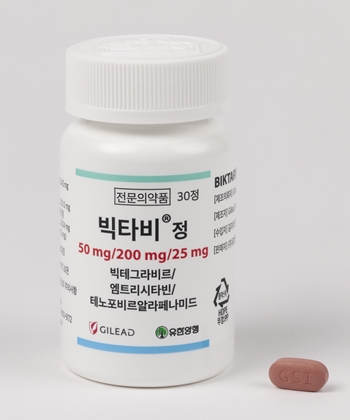
- Biktarvy’s indication expanded to patients 6yrs and older
- by Whang, byung-woo Oct 24, 2024 05:52am
- Pic of Biktarvy The indication for the HIV-1 treatment Biktarvy (bictegravir/emtricitabine/tenofovir alafenamide, B/F/TAF) has been expanded to include children and adolescents aged 6 years and older. Gilead Sciences Korea announced on the 23rd that its Biktarvy has been approved by the Ministry of Food and Drug Safety for the treatment of HIV-1 infection in children or adolescents 6 years of age and older. The approval allows Biktarvy’s use in adults and pediatric patients aged 6 years and older weighing 25 kg or more who are antiretroviral treatment-naïve or who have achieved stable viral suppression (HIV-1 RNA
- Company
- Reimb of the dyslipidemia drug Leqvio at a halt?
- by Eo, Yun-Ho Oct 24, 2024 05:52am
- The dyslipidemia drug that received industry attention as a first-in-class siRNA drug is facing difficulties in obtaining insurance reimbursement coverage in Korea. According to Dailpharm’s coverage, Novartis Korea's Leqvio (inclisiran) applied for new drug reimbursement after receiving approval from the Ministry of Food and Drug Safety in June, but during the Health Insurance Review and Assessment’s review process, the company and the government, especially the medical community and the government, were found to have major differences in opinion in setting the reimbursement standards. The government is considering reimbursing the drug for the rare disease, familial hypercholesterolemia, not for the treatment of dyslipidemia, the main indication. This is similar to when the PCSK9 inhibitor Repatha (evolocumab) was initially listed. Furthermore, as Leqvio’s competitor Repatha, which is in the same therapeutic position, is already being reimbursed, it is possible that the government feels delaying Leqvio’s reimbursement as long as possible would not pose a problem. However, it is worth noting that this does not take into account the fact that Leqvio is administered by a healthcare provider in a hospital just twice a year. This will improve adherence, not just because of the reduced number of doses, but because it is administered by a healthcare professional in a hospital rather than by self-injection. In fact, 78.4% of patients in the study population, including those with ASCVD who received Leqvio for up to 6.8 years or more, achieved their target LDL-C levels. In the US real-world study, patients with ASCVD, including myocardial infarction, who were fully adherent had a 27% lower risk of major adverse cardiovascular events (MACE) compared to those who were not fully adherent. In addition, the fully adherent group had lower annual healthcare costs than the less adherent group, confirming that high adherence not only reduces the risk of recurrent cardiovascular events but also the economic burden of ASCVD patients. Cardiovascular disease accounts for 18% of all deaths in Korea. Over the past decade, this rate has been rising steadily, and the incidence of cardiovascular disease has recently spread to affect younger people. In a market that amounts to KRW 1 trillion for statin and ezetimibe combination drugs alone, it is estimated that the financial expenditure being spent on LDL-C lowering alone would be between KRW 1.5 trillion to KRW 2 trillion in Korea if we add the financial expenditure for statins and pcsk9 inhibitors. However, the LDL-C target achievement rate for ASCVD patients in Korea is a mere 24%. At the policy session of the Korean Society of Cardiology's Fall Meeting that was held on the 18th, Jang-hwan Bae, Chief of Good Samsun Hospital, mentioned Leqvio while pointing out the issue of restricting the reimbursement standards for new drugs, “Leqvio, which is approved in Korea as a bi-annual treatment, is currently being discussed for reimbursement, but just for familial hypercholesterolemia.” Meanwhile, Repatha is reimbursed in 41 countries, including major countries, and Leqvio is reimbursed in 39 countries.
- Company
- Moderna’s keyword for post-COVID vaccination is ‘RWE’
- by Whang, byung-woo Oct 23, 2024 05:50am
- With the COVID-19 pandemic transitioning to the post-COVID-19 era, Moderna is putting forward ‘real-world evidence (RWE)’ as the keyword for its vaccines. As the seasonal vaccination of COVID-19 vaccines has become the norm, the company has been promoting the accumulated effectiveness and safety of its vaccines. (from the left) Jae-Kap Lee, Professor of Infectious Disease at Hallym University Kangnam Sacred Heart Hospital, Piyali Mukherjee, Executive Vice President, Medical Affairs, Moderna Asia Pacific Since the pandemic, the Korea Disease Control and Prevention Agency (KDCA) has designated COVID-19 as an infectious disease that requires annual vaccination along with influenza (flu). As a result, this year, as in previous years, the KDCA is recommending people aged 65 and older, who are at higher risk of both COVID-19 and influenza, receive both vaccines at the same time. However, there is still a lack of awareness of the disease compared to the flu. According to a survey of 1,003 adults in Korea, only 14.5% of the respondents perceived COVID-19 vaccination as important to protect their health, which is over 3 times lower than the 54.2% for the flu. COVID-19 awareness lower than flu, emphasizing the need for vaccination At a conference hosted by Moderna Korea on the 22nd, Jae-Kap Lee, Professor of Infectious Disease at Hallym University Kangnam Sacred Heart Hospital, emphasized the lingering dangers of COVID-19. “COVID-19 is a dangerous disease that causes higher hospitalization and mortality rates than influenza due to the constant rise of new variants,” said Professor Lee. “Among elderly patients, hospitalization rates for COVID-19 were 5 times higher than influenza, and in-hospital mortality rates were 3 times higher for COVID-19 than influenza among those with underlying medical conditions.’ Given this, Lee believes high-risk groups, including those aged 65 and older, should be vaccinated against COVID-19 alongside the flu to protect them from health deterioration and disease burden. Moderna is supplying the COVID-19 vaccine, ‘Spikevax JN,’ in line with the government's 2024-2025 seasonal vaccination plan, which began on the 11th of this month. Jae-Kap Lee, Professor of Infectious Disease at Hallym University Kangnam Sacred Heart Hospital In Korea, there are currently 7.55 million doses of COVID-19 vaccine available in the country for this season, including 5.23 million doses of Pfizer, 2 million doses of Moderna, and 320,000 doses of Novavax vaccines. With multiple COVID-19 vaccine options, Moderna emphasized the accumulation of real-world experience (RWE) as its vaccine’s strength. ‘With more than 1 billion doses of Moderna's COVID-19 vaccine supplied, its RWE continues to confirm its effectiveness and safety. In a real-world study evaluating its COVID-19 prevention effect, the Moderna vaccine booster arm reduced hospitalization rates by 89%,’ said Piyali Mukherjee, Executive Vice President, Medical Affairs, Moderna Asia Pacific. She added, “Moderna’s Spikevax is available in single-dose vials to help both healthcare providers and patients in the country, increasing the likelihood of required dose administration and reducing the chance of contamination. Moderna's vaccine is the only mRNA vaccine manufactured in Korea in partnership with Samsung Biologics.” Most importantly, Vice President Mukherjee said, Moderna's vaccine has proven its value in the current situation where concurrent vaccination for COVID-19 and flu is recommended. “In a Phase III study evaluating the combination of a quadrivalent influenza vaccine and Moderna's COVID-19 vaccine, the combination resulted in a high immune response and a tolerable safety profile.” ‘Flu+COVID-19’ combo vaccine is on the horizon...domestic clinical trials to start next March Another hot topic related to COVID-19 vaccination at the event was the rise of a ‘combo vaccine’ that protects against both flu and COVID-19. Moderna has completed clinical trials on the combo vaccine and plans to submit data to regulatory authorities in Europe and the United States, which is expected to be a game changer in the future. In Korea, the company plans to start enrolling patients for a bridging trial in March next year. “The combo vaccine will first be approved abroad, and patient enrolment in Korea will start in March next year. We expect discussions on approval will take place after 2-3 years of clinical trials,” said Professor Lee. “Many companies are conducting clinical trials on mechanisms that prevent both COVID-19 and influenza at the same time with interest.” While cost remains an issue in the long term, there is no doubt that a combo vaccine that protects against both COVID-19 and flu would be a game-changer, said Lee. “Currently, two doses are administered separately, but the combo vaccine is only one dose. When you look at the cases of children, the market share changes when the combo vaccine comes out,’ he said, adding, ’If the price of the combo vaccine becomes affordable for the government to supply, I don't think there will be much of a problem with its marketability.”
- Company
- "Multiple myeloma dynamics require changes to reimb strategy
- by Whang, byung-woo Oct 22, 2024 05:51am
- Youngil Koh, Professor of the Department of Hemato-Oncology at Seoul National University Hospital "Multiple myeloma is a cancer type that has a great ripple effect depending on new drugs provided in a certain environment. Reimbursement of multiple myeloma treatment requires discussion following a thorough evaluation of the impact of the treatment depending on the treatment environment." Multiple myeloma is one of the cancer types with increased treatment options following new drug entries. There are concerns about extending the relapse period and progression-free survival (PFS) as the number of treatments increases due to relapses. However, the discussion for reimbursement is hindered by cost issues. Youngil Koh, Professor of the Department of Hemato-Oncology at Seoul National University Hospital, emphasizes the importance of discussing appropriate disease-specific environments. According to Koh, the development of new drugs for blood cancers is active because of disease characteristics. Because cancer cells tend to exist in the blood and it is easy to obtain samples, the research is relatively simple. Understanding of blood cancer yields significant results compared to solid cancers. "Almost all new drugs begin from blood cancers, including TKI, therapeutic antibody, bispecific antibody, and ADC, and expand to solid cancers. Bispecific antibodies and ADCs are used as the standard treatment for blood cancers and expand their indications to solid cancers," Koh said. In South Korea, a bispecific antibody treatment, Tecvayli (teclistamab), is available for treating multiple myeloma. This drug was approved in July. The use of Tecvayli is limited because it is not reimbursed, but the expansion of market presence is expected following the announcement of long-term follow-up research results of the drug's clinical trial, MajesTEC-1, at the American Society of Clinical Oncology (ASCO 2024) meeting. The results of evaluating the efficacy of Tecvayli in 165 study participants at 30.4 months interim follow-up showed that Tecvayli reduced tumor sizes by 63% (overall response rate, ORR) in patients who had failed or were non-responsive to third-line treatments or higher. 46.1% of the patients reached complete remission (CR). The study confirmed consistent, long-term clinical effectiveness and positive safety profile. "The 30-month follow-up outcome did not differ from the data presented in 2022; therefore, it is significant that we have confirmed the anticipated outcome," Koh said. "Specifically, 4 out of 10 patients showed great responses and maintained response over two years." "We have observed that the real effects observed in 30-50 patients administered with the drug at the Seoul National University Hospital did not differ greatly from the research," added Koh. "1/3 of the patients benefited from the treatment, and close to half experienced great responses." In conclusion, Koh says that the result should be highly regarded because Tecvayli's long-term follow-up data demonstrated that patients showed a significantly long response period after almost two-years of treatment. Will Tecvayli, demonstrating its long-term effects, be adminstered earlier in the treatment course? Based on the assumption that there are no differing opinions about the effect of Tecvayli, the question is 'when' to use the drug. There are concerns about using the good drug first or last, regardless of disease. However, multiple myeloma requires a more careful approach because the treatment order is particularly important. Koh says it is difficult to determine at this point, but Tecvayli is likely to be placed earlier in order since the data supporting its use of Tecvayli in earlier treatment course are now available. "Tecvayli is the only bispecific antibody to be used for the treatment of multiple myeloma in South Korea and it targets BCMA, which the conventional treatments haven't targeted," Koh said. "Based on the clinical data of Tecvayli used in combination with already effective treatments that are currently used, Tecvayli is likely to be employed earlier in the treatment and will be able to extend overall survival," Koh said. However, Koh assessed that it is too early to mention whether bispecific antibody, known as the next-generation treatment, or CAR-T therapy should be placed earlier. "The positions of bispecific antibody and CAR-T for treating multiple myeloma have not been established yet. We now know that two treatments successfully treat multiple myeloma, but it is early to determine which one is superior. Upcoming clinical data will determine their positions," Koh emphasized. "Multiple myeloma is highly dynamic…changes to reimbursement strategy should be considered" Besides the Tecvayli effect, the dilemma for new drugs is the cost. Patient burden increases when high-cost drugs are not covered by reimbursement. Since multiple myeloma treatment tends to use 2-3 treatments in combination, the government is hesitant to opening the door to reimbursement. Regarding this issue, Koh advises that rather than simply comparing the cost of the drug, a reimbursement strategy reflecting the characteristics of multiple myeloma should be discussed. "The dynamic of treatments for multiple myeloma is changing due to new drugs, and the disease is greatly influenced by the type of new drugs and the type of reimbursement. We need to discuss reimbursement after anticipating the potential impact of reimbursement on overall treatment outcomes," Koh explained. "The landscape of multiple myeloma is diverse and constantly changing; therefore, instead of simply comparing costs, the government can strategize better reimbursement plan taking into account various outcomes," Koh said. Koh stated that we need to discuss patient access to clinical trials while reimbursement for new drugs is limited. "New drugs are being developed faster than the reimbursement process. It is inevitable that patients cannot benefit from new drugs because reimbursement cannot cover all," Koh said. "In other words, drugs are available at clinical stages, so we could discuss increasing patient access to new drugs."
- Company
- Will combination therapies for cancer be reimbursed in KOR?
- by Whang, byung-woo Oct 21, 2024 05:49am
- As the government has begun to prepare the principles for the reimbursement review of combination therapies that use new anticancer drugs, attention is being paid to whether the discussion will progress further. According to industry sources, the Health Insurance Review and Assessment Service recently held a Cancer Disease Deliberation Committee meeting and decided to prepare deliberation principles to discuss whether to approve benefits for major combination therapies. The decision is in line with the growing calls for a change in the reimbursement paradigm for prescribing anticancer drugs based on accumulated evidence on ‘combination therapies’ between treatments from various clinical studies. Recently, multinational pharmaceutical companies have been seeking the reimbursement of combination therapies using new anticancer drugs, calling for an institutionalized process. When considering reimbursement for combinations of non-reimbursed new drugs and reimbursed chemotherapy drugs, the industry has suggested that discussions on previously reimbursed drugs should be reserved and only the non-reimbursed drugs should be discussed. A case in point is AstraZeneca's immuno-oncology drug Imfinzi (durvalumab), the reimbursement of which had been discussed for biliary tract cancer last year. At the time, CDDC only approved gemcitabine and cisplatin in combination with chemotherapy (the GemCis regimen) for first-line treatment of biliary tract cancer, while leaving Imfinzi non-reimbursed. The government will discuss setting a deliberation principle where a drug, which is already reimbursed, is used with a non-reimbursed new drug as part of combination therapy and should continue to be reimbursed without further discussions. This can be observed in the results of the 7th CDDC Review, which reviewed the combination of ‘endocrine therapy’ and ‘Verzenio (abemaciclib)’ for the treatment of early breast cancer. The outcome of the deliberations was to keep the previously reimbursed adjuvant endocrine therapy as is and make the newly added Verzenio available on a ‘100% coinsurance’ basis, reducing the cost burden on the patients. In other words, it means that the process will be simplified by allowing the reimbursement of existing treatments within the combination to be recognized. However, these principles are not automatically applicable to all new combination therapies, and as it leaves the existing framework in place, it is far from the improvements to the new drug approval approaches the industry had hoped for. Nevertheless, it is positive as it has opened the door to further discussions. There are also expectations that such discussions will lead to solutions for ‘new drug+new drug’ combination therapies. A pharmaceutical industry official said, “It is still a drug-by-drug approach, so it's not a one-size-fits-all approach, but it's positive that the discussions have been officially made. We understand that KRPIA and others are also having discussions on what kind of processes will be required for the reimbursement of new drugs for combination therapies in the future,’ “With the number of combination therapy cases increasing, there is currently no set process for how applications should be submitted for listing and how they should be reviewed. We are looking forward to the various approaches that may be developed through discussions as individual cases have come to light.”