- LOGIN
- MemberShip
- 2025-12-21 21:44:27
- Company
- Leclaza’s new trial data shows improved OS
- by Son, Hyung Min Jan 09, 2025 05:57am
- The Leclaza plus Rybrevant combination achieved statistically significant overall survival (OS) results. Johnson & Johnson expects Leclaza plus Rybrevant to extend OS by more than a year compared to Tagrisso monotherapy. The positive OS outcome for the combination strengthens its potential to become the first-line standard of care for EGFR-positive NSCLC. On the 7th, Johnson & Johnson announced top-line OS results from the Phase III MARIPOSA study, which evaluated the efficacy of the combination of Leclaza plus Rybrevant in patients with locally advanced or metastatic NSCLC. Leclaza is a third-generation tyrosine kinase inhibitor (TKI) targeting exon 19, and exon 21 (L858R) in EGFR-positive NSCLC that was developed by Yuhan Corp. Johnson & Johnson acquired global rights to Leclaza and is conducting clinical trials for the drug in combination with its targeted therapy option, Rybrevant, which targets exon 20 and the MET mutation. The recently published OS results showed that Leclaza plus Rybrevant was superior to Tagrisso monotherapy. Johnson & Johnson explained that Leclaza plus Rybrevant extended median OS by more than a year compared to Tagrisso alone, which was a statistically significant result. As Tagrisso achieved a median OS of 38.6 months in the FLAURA study that became the basis of its approval, the OS for Leclaza plus Rybrevant is expected to have exceeded 50 months. This is progress over previous clinical data, which demonstrated efficacy in the primary endpoint of PFS, but only a favorable trend over Tagrisso in the secondary endpoint of OS. OS is one of the most important indicators in determining the clinical value of an anticancer drug. OS is the overall survival period from the time a patient starts treatment until death. OS also includes patients who die of non-cancer-related causes, such as side effects and other complications. In the case of PFS, PFS is the length of time that a patient survives with cancer that has not progressed, i.e., the tumor has not increased in size while receiving treatment. In other words, while PFS is a measure of how well a new treatment can slow the progression of cancer, OS is a measure of how well it can prolong survival. If the Leclaza plus Rybrevant is ultimately to have an effect in improving PFS and OS, it could become the standard of care for EGFR-positive non-small cell lung cancer. Johnson & Johnson succeeded in receiving FDA approval for Leclaza plus Rybrevant in August of last year based on the results of the MARIPOSA trial. In December last year, Johnson & Johnson received approval in Europe as well. The approval was based on clinical results that Johnson & Johnson presented at the European Society for Medical Oncology 2023 Annual Congress (ESMO 2023). The results showed a median progression-free survival (PFS) of 23.7 months in the Leclaza plus Rybrevant combination arm and 18.5 months in the Leclaza monotherapy arm, compared to 16.6 months in the Tagrisso monotherapy arm. “Achieved results with targeted therapy+ targeted therapy”...ignites competition between combination therapies” The competition between combination therapies has also started in earnest in the market for the first-line treatment of EGFR-positive NSCLC. Currently, AstraZeneca is defending the market with Tagrisso plus platinum-based chemotherapy, which is approved for the first-line treatment of EGFR-positive NSCLC. However, platinum-based chemotherapy is categorized as an option for use after a patient develops resistance to conventional targeted therapies. This is why some have argued that using platinum-based chemotherapy as a first-line option could lead to a shortage of later-line therapy options after developing resistance. The downside to the use of the Leclaza plus Rybrevant combination is that it may be less convenient to administer. All EGFR-positive targeted therapies, including Leclaza, Tagrisso (third generation), Boehringer Ingelheim’s Giotrif, Pfizer’s Vizimpro (second generation), Roche’s Tarceva, and AstraZeneca’s Iressa (first generation), are oral formulations. However, Rybrevant is an intravenous (IV) formulation that requires clinic visits every three weeks. This may not be convenient for patients with NSCLC. To address the issue, Johnson & Johnson has developed a subcutaneous (SC) formulation of Rybrevant and has been studying the formulation in combination with Leclaza. The subcutaneous formulation can be administered in as little as 10 minutes, significantly reducing dosing time for the patients. In recently published clinical trial results, the combination of the subcutaneous formulation of Rybrevant and Leclaza demonstrated similar outcomes to the intravenous (IV) formulation of Rybrevant plus Leclaza. Infusion-related adverse events were lower in the Rybrevant SC+ Leclaza arm. “Leclaza+Rybrevant delivered clinically significant results without chemotherapy,” said Yusri Elsayed, Global Head of Oncology at Johnson & Johnson. ”Extending median overall survival by more than a year can be a game-changer in the NSCLC treatment landscape.”
- Company
- Vabysmo approved for retinal vein occlusion macular edema
- by Whang, byung-woo Jan 09, 2025 05:56am
- Pic of Vabysmo Roche Korea announced on the 8th that Vabysmo has been approved by the Ministry of Food and Drug Safety (MFDS) for the treatment of visual impairment due to macular edema secondary to retinal vein occlusion. With the approval, Vabysmo is now approved for 3 indications in Korea, including as a treatment for ▲neovascular (wet) age-related macular degeneration; ▲visual impairment due to diabetic macular edema; and ▲visual impairment due to macular edema secondary to retinal vein occlusion. Retinal vein occlusion is the second leading cause of blindness due to retinal vascular disease. It primarily affects people over the age of 60 and can cause sudden vision loss. Retinal vein occlusion is divided into two main types: branch retinal vein occlusion, which occurs when one of the four smaller branches of the main central retinal vein becomes blocked, and central retinal vein occlusion, which occurs when the central retinal vein in the eye becomes blocked. The approval of this indication expansion is based on results from the global Phase III BALATON and COMINO clinical trials, which included over 1,200 patients with macular edema secondary to retinal vein occlusion. In BALATON and COMINO trials, Vabysmo met the study's primary endpoint by demonstrating non-inferior visual acuity improvement compared to the control group as measured by best-corrected visual acuity (BCVA) at week 24 in patients with branch retinal vein occlusion (BRVO) and central retinal vein occlusion (CRVO). Additional long-term data from up to 72 weeks of follow-up showed that more than 57% of patients in the BALATON study and more than 45% of patients in the COMINO study were able to extend the treatment interval to three- or four-month intervals. In the BALATON and COMINO trials, Vabysmo was well tolerated, with a safety profile consistent with previous studies. The most common adverse event was conjunctival hemorrhage (3%), with a comparable safety profile across study arms. “This indication expansion is significant because it allows Vabysmo, the first bispecific antibody treatment for ophthalmic diseases, to contribute to the treatment of a broader spectrum of retinal diseases, in the current situation where it is becoming increasingly important to treat ophthalmic diseases due to the aging population and increase in chronic diseases,” said Ezat Azem, General Manager of Roche Korea. “We will continue to work with key stakeholders, including the government and academia, to support healthier lives for Korean patients with retinal diseases by providing treatments for conditions that can cause blindness.”
- Company
- Krazati receives orphan drug designation in Korea
- by Eo, Yun-Ho Jan 09, 2025 05:56am
- The second KRAS inhibitor 'Krazati' has been designated as an orphan drug in Korea. The Ministry of Food and Drug Safety (MFDS) recently announced the news through the first orphan drug designation announcement of the new year. Specifically, Krazati is indicated for 'locally advanced or metastatic non-small cell lung cancer (NSCLC) with KRAS G12C mutation who have received at least one prior therapy. BMS's Krazati (adagrasib) received accelerated approval from the U.S. FDA in December 2022. It is the second KRAS inhibitor to be approved, following Amgen's Lumakras (sotorasib), which was approved in 2021. The development of KRAS-targeted anticancer drugs comes nearly 40 years after the oncogene KRAS was first discovered. Amgen and BMS are in a fierce race to capture the new market. Lumakras and Krazati have many similarities in terms of target mutation and indication. Both target the G12C variant of KRAS, and were first approved for non-small cell lung cancer. The companies are also conducting combination trials with drugs that have different mechanisms of action, either developed in-house or acquired through collaborative research. Krazati's first approval was based on results from the enrollable cohort from the Phase II KRYSTAL-1 study, and the company disclosed top-line results from a confirmatory Phase III study last year. The study evaluated Krazati versus docetaxel in 301 previously treated patients with KRAS G12C mutated locally advanced or metastatic NSCLC. The study enrolled patients with KRAS G12C-mutated locally advanced or metastatic NSCLC who had been previously treated with platinum-based chemotherapy and anti-PD-1/PD-L1 immunosuppressive agents. Patients were randomized in a 1:1 ratio to receive Krazati or docetaxel. The primary endpoint was progression-free survival (PFS) as assessed by BICR. At 9.4 months of follow-up, the primary endpoint was met with a median PFS of 5.49 months for Krazati compared to 3.84 months for docetaxel, a 42% reduction in the risk of disease progression or death.
- Company
- Wegovy vs Mounjaro in KOR…who's the winner?
- by Moon, sung-ho Jan 09, 2025 05:56am
- As more people are living with obesity in the world, obesity treatment is gaining popularity. According to the World Obesity Federation report, more than half of the world's population in 2035, 10 years from now, will be categorized as overweight or obese. South Korea is projected to have a similar rate. At the end of last year, Novo Nordisk's obesity drug 'Wegovy (semaglutide),' which gained popularity and was in short supply in the global market, was finally introduced to clinical practices in South Korea. After that, new drugs with significant weight-loss effects are being introduced into South Korea, indicating a shift in the paradigm of obesity treatment. The companies have applied for expanded indications for these drugs, influencing clinical areas. Prodouct photo of According to pharmaceutical industry sources on January 6, Novo Nordisk Korea has been supplying 'Wegovy Prefilled Pen Inj' to clinical practices since mid-October last year. Wegovy received domestic marketing authorization in April with indications to aid weight-loss overweight patients who have a Body Mass Index (hereafter referred to as BMI) of 30kg/m2 or higher or those who are overweight with early BMI of 27kg/m2 or higher and below 30kg/m2 and having one or more weight-related accompanying diseases. Additionally, in July 2024, Wegovy also receive approval for the indication to reduce risks of major cardiovascular events (death from cardiovascular diseses, non-fatal cardial infarction, or non-fatal cerebral strok) in overweight or obese patients with early BMI of 27 kg/m² or higher with cardiovascular diseases. Upon the launch of Wegovy, Novo Nordisk Korea actively worked to secure market dominance in the Korean obesity treatment market, using about 80 sales and marketing employees. As a result, Wegovy is currently being used in medical clinics as a non-reimbursable drug. Patients pay an average cost of KRW 700,000-800,000 per month for treatment. "Japan's drug price seems to be the world's lowest, but it is covered by insurance. It has been launched as the lowest price globally among non-reimbursed drugs," Chul Jin Lee, President of the Korean Society for the Study of Obesity (Joeun Family Health Clinic), said. "It is likely that the company has considered the potential launch of Mounjaro (tirzepatide) in Korean clinical practices." Wegovy's company seems to be attempting to dominate the market by entering the domestic clinical field ahead of Mounjaro. The industry's interest is now on the launching date of 'Mounjaro,' known as Wegovy's rival. Lily Korea plans to introduce the drug to clinical practices in South Korea this year. In addition to Mounjaro's approval for type 2 diabetes, Lily Korea received extended approval for the drug as an adjuvant therapy for chronic weight control, which is similar to Wegovy. Although it is being sold in the market for obesity treatment as the product name 'Zepbound,' Mounjaro will be used for treating diabetes and obesity in South Korea. Regarding this, Lily's recent announcement of the top-line results of the open-label SURMOUNT-5 Phase 3 clinical trial draws attention. This study directly compared the effects of Mounjaro to Wegovy. According to the results presented, patients treated with Mounjaro had greater weight loss effects compared to those treated with Wegovy. This finding indicates that Mounjaro is superior in a one-on-one comparison to Wegovy. In the clinical study involving 751 patients who are obese or overweight without diabetes, patients treated with Mounjaro for 72 weeks had a weight loss of 22.67kg, which is an average loss of 20.2% of the body weight. During the same period, patients treated with Wegovy had a weight loss of 13.7% (14.96kg). When the weight loss range was compared, Zepbound showed about 47% superior effects than Wegovy. Consequently, when Mounjaro becomes available in the Korean market, Wegovy will likely face a short-lived 'popularity.' "Mounjaro in the form of vial is under consideration of domestic approval," Lee said. "Mounjaro's yearly cost is about KRW 3 million less than what Wegovy costs. Moreover, the drug price of vial formation saw a 50% reduction in the United States. When it launches in South Korea after obtaining approval, Mounjaro will likely priced significantly less. For this reason, clinical practices are closely watching Mounjaro." "When vial formation becomes available, doctors prefer using those than pen types," Lee added. "A weekly vial package treatment regimen would be optimal." Due to Wegovy and Mounjaro's success, GLP-1 emerged as the R&D trend in the domestic and foreign pharmaceutical and biotech industries. Recently, the FDA granted approval for Zepbound, containing a similar active ingredient to Mounjaro, for sleep apnea. In addition to its diabetes and obesity indications, the extended indication of sleep apnea suggests an increased volume of usage. Also, an extended indication is likely approved in South Korea. Companies witnessing these successes are evaluating the possibility of metabolic dysfunction-associated steatohepatitis (MASH) treatment since GLP-1 improves insulin secretion and sensitivity, improving blood glucose control. Because MASH is caused by fat buildup in the liver of people who consume little or no alcohol, weight loss can have a positive effect on patients. For this reason, pharmaceutical companies have determined that GLP-1 can be a treatment for MASH, alongside diabetes and obesity, and are currently conducting clinical trials. The same goes for Wegovy and Mounjaro's active ingredients, semaglutide and tirzepatide. Novo Nordisk and Lily are assessing the clinical utility of those drugs in patients with MASH, conducting phase 2 and phase 3 clinical trials, respectively. The industry is anticipating potential extended indications. Additionally, survodutide, under development by Boehringer Ingelheim, demonstrated clinical utility in a phase 2 trial, emerging as a new drug candidate for MASH. The biotech industry in South Korea is also considering the possibility of new GLP-1 drugs. Many companies have begun clinical studies. The outstanding companies are ProGen and D&D Pharmatech. ProGen is gaining attention for its new drug development in diabetes and obesity fields. The company is developing 'PG-102,' which works bi-specifically by binding GLP-1·GLP-2. ProGen's new drug candidate received approval from the Ministry of Food and Drug Safety (MFDS) for conducting a domestic phase 2 trial. ProGen aims to maximize the effects, such as improving intestine function, glucose uptake in adipose tissue, and alleviating chronic inflammation by targeting both GLP-1 and GLP-2. Kun-Ho Yoon, Chief Medical Officer of Progen (Endocrinology Specialist), says the significance of the study is that "Since there have been no new drug candidates that simultaneously target both GLP-1 and GLP-2, ProGen's 'PG-102' can be a first-in-class candidate treatment." D&D Pharmatech is conducting clinical trials for its GLP-1 agent for various fields, including MASH, Parkinson's disease, and dementia. Last year, the company initiated a Phase 2 trial after receiving the FDA approval of its Phase 2 trial Investigational New Drug (IND) application. The Phase 2 trial is being conducted in 10 clinical trial centers, and the trial involves 68 patients who are overweight or obese with accompanying MASH. The Korean clinical practices are closely watching the D&D Pharmatech's achievements. "D&D Pharmatech has GLP-1 and GLP-2 bi-specific agents and amylin-based products," Lee said. "The company has a competitive edge, especially having a proprietary platform for switching an agent to oral formation alongside having injectable." "Regarding developing a GLP-1 formation, the key to success is which company could diversify with lesser cost," Lee remarked. "The success in the market competition will be determined by providing various clinical benefits at lower prices for injectable, vial, and oral formations," Lee projected.
- Company
- Sales of Flu drug Tamiflu did not fare so well last year
- by Nho, Byung Chul Jan 08, 2025 05:53am
- The oseltamivir-based flu treatment market, commonly represented by Tamiflu, is on a vertical decline after peaking in sales in 2023. The market for related preparations was valued at KRW 35.6 billion in 2023, the largest in 5 years. By 3Q 2024, the oseltamivir market posted sales of KRW 6.2 billion; even when the sales of the fourth quarter are combined, it will be difficult to realize the KRW 10 billion mark. However, given how flu alerts were issued from December last year to January this year, a spike in the drug’s sales is expected during the period. The overall market for related ingredients has remained at the level of KRW 23.1 billion in 2019, and after reaching a low of KRW 10.5 billion in 2020 and KRW 339 million in 2021. The market recovered to KRW 20.9 billion in 2022 and reached KRW 35.6 billion in 2023. The market for related therapeutics shrank significantly during the peak of the pandemic due to the impact of COVID-19 vaccination and strict personal hygiene such as wearing masks and disinfecting hands. Oseltamivir is one of more than 20 products competing in the market for the treatment of influenza A-B virus infections. Roche's Tamiflu is the undisputed leader in the market, with sales of about KRW 2.6 billion through the third quarter of last year. That's down sharply from 2023 when it generated KRW 15.3 billion in sales. Tamiflu's performance in 2019-2020-2021-2022 had been KRW 7.4 billion-4 billion-137 million-14.1 billion, respectively. In second place is Hanmiflu Cap, which sold KRW 1.6 billion by the third quarter of 2024, a sharp drop from KRW 7.7 billion in 2023. Hanmiflu's performance in 2019-2020-2021-2022 is in the range of KRW 4.8 billion-KRW 1.7 billion-KRW 29 million-KRW 2.4 billion. Yuhan Corp’s Yuhan N-flu and Chong Kun Dang’s Tamivir ranked third and fourth with sales of KRW 490 million to KRW 470 million through the third quarter of 2024, respectively. Comyflu (Kolon Pharmaceutical), Seltaflu (Vivozon Pharm), and Oseltawon Cap (Daewon Pharmaceutical) followed, with sales in the range of KRW 100-400 million in the same period, down sharply from the KRW 1.2-1.8 billion in 2023. Kuhnflu (Kuhnil Biophamr), Hanaflu Cap (Hana Pharm), and Shinpoong Flu (Shin Poong Pharm) have been generating sales between KRW 30 million and KRW 80 million until the third quarter of last year. Oseltamivir is taken twice a day for five days within two days of symptom onset, regardless of food intake. The treatment is available for newborns starting at 2 weeks of age, with a recommended dose of 3 mg per kg for children under 1 year of age. Prophylaxis is approved for persons 1 year of age and older and is taken once daily for 10 days at a dose as directed by a physician within 2 days of contact with an infected person. Common adverse reactions include nausea, vomiting, and headache (>10%); if a gastrointestinal disorder occurs, taking it with food could be helpful. Patients should not discontinue the medication at their discretion and should receive guidance to fully take the medication as prescribed. NSAIDs and acetaminophen do not affect the effectiveness of anti-influenza antivirals and may be taken together. However, aspirin should be avoided if a child is infected with influenza and has a fever. Aspirin can cause Reye's Syndrome, a condition that can cause severe vomiting, convulsions, acute encephalopathy, fatty degeneration, and death in children with the virus.
- Company
- J.P. Morgan selects ADC and obesity as big deal keywords
- by Moon, sung-ho Jan 08, 2025 05:53am
- With the opening of the 'J.P. Morgan Healthcare Conference', which attracted much attention last year with domestic pharmaceutical and biotech companies announcing the achievement of 'big deals,’ approaching, attention is gathering on what results will be announced this year. The keywords of this year's event are glucagon-like peptide-1 (GLP-1)--based obesity drugs and antibody-drug conjugates (ADCs), which have risen as hot topics in the global pharmaceutical and bio market. At the event, domestic pharmaceutical and biotech companies will be presenting their portfolios and holding face-to-face meetings. #According to industry sources on the 6th, the 43rd JP Morgan Healthcare Conference is scheduled to be held in San Francisco, U.S., from January 13 to 16 (local time). The event, which celebrates its 43rd event this year, has served as an opportunity for about 600 domestic and large multinational pharmaceutical companies to share their new R&D achievements and status and discuss the future development of the pharmaceutical and bio industry. Above all, it is an opportunity for domestic pharmaceutical and biotech companies to fulfill their main objectives of ”technology exports” and “forging partnerships.” In particular, at this year's event, in addition to the conference regular Samsung Biologics, Lotte Biologics, and Celltrion will unveil their contract development manufacturing Organization (CDMO) facilities and major business strategies. Among them, Samsung Biologics has always participated in the event since the 2020s and unveiled its major business strategies in the Main Track. This year, the company's CEO John Rim will be the main track presenter and will present its manufacturing facilities (5-8 plants) and antibody-drug conjugate (ADC) portfolio. Celltrion will also participate in the event to showcase its drug development achievements, including its ADC anti-cancer pipeline, as well as its CDMO vision. Celltrion is developing 3 ADC drugs and 3 multi-antibody drugs with the goal of commercializing its first product in 2029. Lotte Biologics, which has set its sights on becoming a CDMO specialist, is expected to announce its plans for the CDMO business and the expansion of its Syracuse ADC production facility under its newly appointed CEO James Park. Lotte Biologics previously announced that it will invest KRW 4.6 trillion by 2030 to own the capability as a global-level biopharmaceutical manufacturing competitor. At the same time, the Syracuse Bio Campus has disclosed plans to invest in ADC production facilities and begin full-scale production this year. Along with domestic CDMOs, bio companies that are challenging new drug development also registered and put their names on the event lineup. Among them, Onconic Therapeutics, a subsidiary of Jeil Pharmaceutical, which launched the P-CAB class gastroesophageal reflux disease drug Zaqbo (zastaprazan) last year, will also participate in the event. Onconic Therapeutics will use the JP Morgan Healthcare Conference to focus on strategic meetings with global pharmaceutical companies and investors. In particular, the company plans to accelerate the global market entry of its targeted anti-cancer drug Nesuparib with Zaqbo. “The JP Morgan Healthcare Conference will be an important opportunity to showcase our new drug pipeline and technology to the global market and create new collaboration opportunities,” said a representative from Onconic Therapeutics. “As we excluded the market value of Nesuparib from the public offering price during the KOSDAQ listing process, leaving new shareholders’ interests untouched, we look forward to a full-scale reassessment and valuation of the company through this event.” Bridge Biotherapeutics has been officially invited to make a corporate presentation. The presentation will highlight the company's growth strategy, including BBT-877, its lead candidate for idiopathic pulmonary fibrosis. BBT-877 is in the later stages of a global Phase 2 clinical trial, with top-line data expected next April. To date, 98 patients, representing more than 75% of the total patients, have completed the 24-week dosing process, and data from all patients in the trial will be finalized within the first quarter of next year. In addition, domestic companies that are developing not only anti-cancer drugs but also obesity drugs, a global drug development trend, will also participate in the event. D&D Pharmatech will present its glucagon-like peptide (GLP-1) based obesity treatment. In November last year, D&D Pharmatech started clinical trials for DD02, an oral GLP-1-based obesity treatment, through its U.S. partner Metsera. Also, Dx&Vx will also be participating in the event to share the progress of its own oral GLP-1 obesity drug currently in development. “As global pharmaceutical companies compete to develop oral GLP-1 therapeutics, interest in our technology is growing,” said a representative from Dx&Vx. ”We look forward to strengthening our global presence at the J.P. Morgan Healthcare Conference and collaborating with various partners to bring better treatment options to patients.”
- Company
- Expansion of NIP needed for 20-valent pneumococcal vaccine
- by Whang, byung-woo Jan 08, 2025 05:53am
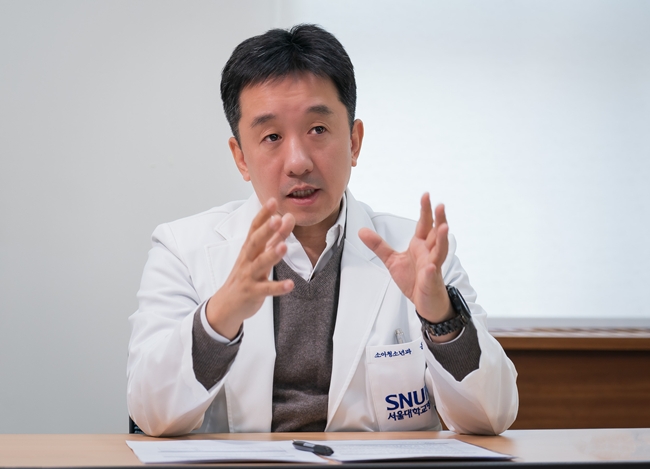
- "Invasive pneumococcal disease remains the most common invasive infection and poses a significant burden. Pneumococcal diseases, such as pneumonia or ear infection, pose significant burden. The new vaccine must cover conventional serotypes as well as newly introduced serotypes to manage the invasive pneumococcal infection and expect an additional reduction." The introduction of the pneumococcal vaccine with the most serotypes in South Korea has brought attention to its preventive effects against pneumococcus and unmet needs for vaccines. Given the availability of vaccines in the National Immunization Program (NIP), there is a heightened interest in the preventive effects of added serotypes. Dr. Ki Wook Yun, Professor of the Department of Pediatrics and Adolescent Medicine at Seoul National University College of MedicineDr. Ki Wook Yun, Professor of the Department of Pediatrics and Adolescent Medicine at Seoul National University College of Medicine, emphasizes the importance of seeking ways to improve preventive effects in terms of society, given the additional effects of newly introduced drugs. According to Dr. Yun, unlike viral infection, bacterial infection cannot be recovered by relying on immunity, requiring antibiotic treatment. Mortality in children has decreased compared to the past, but bacterial infection still needs considerable attention. "Bacterial infection is one of the most burdening diseases in children. The prevalence decreased over time due to vaccine development and environmental improvement. Yet, the disease prevalence is higher than other diseases," Yun explained. "Not only children with immature immunity but seniors are prone to respiratory infections. Consequently, children and seniors are the primary patients for respiratory prevention and treatment." Dr. Yun comments that given these factors, it is crucial to prevent infection through vaccination and to stop it from transitioning to severe stages. Invasive pneumococcal disease remains the most common invasive infection and poses a high disease burden, so the importance of vaccination has been stressed. "Bacterial identification is challenging for infections related to pneumococcus, leading to frequent use of antibiotics. Consequently, patients may experience aftermaths of the treatment," Dr. Yun stated. "Vaccines can prevent these issues and may alleviate antibiotic tolerance by reducing the volume of antibiotic use." The government has included 13-valent and 15-valent pneumococcal vaccines in the NIP for children. From a different view, it remains to be seen what impact of Prevenar 20, a recently approved vaccine containing 20 serotypes, will have. Dr. Yun focuses on newly identified serotypes not included in the 13-valent vaccine as primary causes of infection. "13-valent vaccine alone cannot prevent all serotypes, so vaccines that contain new serotypes may be necessary," Dr. Yun said. "New vaccine must cover conventional serotypes as well as newly introduced serotypes to manage invasive pneumococcal infection and expect additional reduction." "Because Prevenar 20 also met non-inferiority to 13-valent vaccines, and it met immunogenicity requirements set by WHO at the fourth immunization, using the vaccine will likely be similar to the conventional vaccine," Dr. Yun added. "Additional serotypes can also offer disease prevention, so clinical benefits are expected." "The 20-valent pneumococcal vaccine has established sufficient validity for the NIP…establishing mass immunity must be considered" The remaining issue is whether the vaccine will be included in the NIP. While it offers broader prophylaxis than conventional vaccines, its introduction faces cost concerns due to the existing conventional vaccines already being part of the NIP. Dr. Yun analyzes that considering foreign cases, disease burden, and as drug price increases, Prevenar 20 has established sufficient validity for the NIP. "The 20-valent vaccine includes seven additional serotypes compared to conventional vaccines, potentially providing about 40-50% additional prevention against invasive pneumococcal infections. This suggests that the vaccine is more effective than existing ones," Dr. Yun said. "About 70-80% of non-vaccine serotypes causing infections in South Korea are not included in existing vaccines," Dr. Yun stated. "About half of these are serotypes included in the 20-valent vaccine. Consequently, it may be inadequate to keep using existing vaccines." Dr. Yun particularly emphasizes that to maximize the effects of the pneumococcal vaccine, increasing the vaccination rate for mass immunity must be considered. The 13-valent conjugate vaccine previously achieved high vaccination rates and demonstrative high effectiveness. However, a drop in vaccination rates due to new vaccines not being included in the NIP may lead to an increase in invasive infections and pneumonia. "Rather than expecting protection from individual vaccination, we must consider approaches generating society-wise preventive effects. Considering these views, there must be active measures to increase the vaccination rate with new vaccines such as Prevenar 20," Dr. Yun said. Finally, Dr. Yun remarked, "Despite the significant burden of pneumococcal diseases, such as pneumonia or ear infection, a surveillance system has not been established in South Korea." Adding, "The Korea Disease Control and Prevention Agency (KDCA) must address these aspects and implement systematic improvements so that invasive pneumococcal diseases are not overlooked."
- Company
- New drug 'Truqap' for HER2- breast cancer Rx available
- by Son, Hyung Min Jan 08, 2025 05:53am
- Product photo of AstraZeneca Korea'Truqap,' an oral anticancer drug that targets AKT gene mutation, is now available for prescription at general hospitals. According to industry sources, AstraZeneca Korea's Truqap (capivasertib), a treatment for hormone receptor (HR)-positive and human epidermal growth factor receptor 2 (HER2)-negative advanced breast cancer, has passed the drug committees (DC) of tertiary general hospitals, including Samsung Medical Center and Seoul National University Hospital, and medical centers, including Gachon University Gil Medical center, Gangnam Severance Hospital, Korea University ANAM Hospital, Seoul National University Bundang Hospital, and Cha University Bungdang Medical Center. Domestically approved in March 2024, Truqap was launched as a non-reimbursable drug in September of the same year. This drug can be prescribed for combination therapy with fulvestrant following progression on or after an endocrine therapy or recurrence within 12 months after adjuvant therapy. The introduction of Truqap is significant because it offers more second-line treatment options following first-line treatment of HR-positive/HER2-negative breast cancer where there have been unmet needs. HR-positive/HER2-negative breast cancer accounts for 70% of the total breast cancer patients. This drug was demonstrated to be efficacious based on the CAPItello-291 Phase 3 study. The results showed that Truqap improved the median progression-free survival (mPFS) by approximately 2.5-fold compared to fulvestrant alone in patients who failed the first-line treatment following endocrine therapy (ET)±CDK4/6 inhibitor therapy. In detail, the Truqap+fulvestrant combination group had a mPFS of 7.3 months, which is more than double the 3.1 months with fulvestant alone. "Patients with PIK3CA/AKT1/PTEN mutations, accounting for about 50% of patients with HR-positive/HER2-negative breast cancer, may have faster disease progression; therefore, there has been a consistent need for second-line treatment for metastatic breast cancer targeting these mutations," Dr. Kywong Hwa Park, Professor of the Division of Oncology at Korea University ANAM Hospital, explained. "In metastatic breast cancer, patients who achieve complete recovery with a first-line treatment is rare, and most patients fail treatments, leading to the second-line treatments or more. The mutation targeted by Truqap commonly metastasizes to various organs, so we anticipate a positive outlook with this medication," Dr. Park said.
- Company
- Twice yearly HIV drug 'lenacapavir' receives ODD
- by Eo, Yun-Ho Jan 07, 2025 06:05am
- Product photo of Sunlenca Twice yearly injectable 'lenacapavir' for HIV prevention has been designated as an orphan drug in South Korea. The Ministry of Food and Drug Safety (MFDS) recently announced this through the new year's first orphan drug designation notification. The drug is indicated 'In combination with other antiretroviral therapy, for treatment of patients with multidrug-resistant HIV-1 infection for whom cannot be treated with antiretrovirals.' This drug, marketed under the product name as 'Sunlenca,' is a first-in-class long-acting HIV-1 capsid inhibitor that is subcutaneously administered every six months. It was approved in the United States and Europe in 2022 and has been prescribed. The current HIV treatment regimen requires daily oral administration of antiretrovirals. As long-acting agents become available, the treatment frequency has been extended to two or six months. Sunlenca offers not only HIV treatment but also 'prevention.' In September 2024, this drug's developer, Gilead Sciences, announced the second interim result of lenacapavir's Phase 3 PURPOSE2 trial. The result has shown that lenacapavir reduced HIV infection by 96% compared to baseline HIV prevalence (HIV). Only two cases occurred among 2180 study participants, suggesting that 99.9% of the participants in the lenacapavir-treated group had not been infected with HIV. The PURPOSE 2 study is the second key Phase 3 trial evaluating the efficacy of twice-yearly lenacapavir as a pre-exposure prophylaxis (PrEP) used to prevent HIV. In June 2024, Gilead Sciences concluded the double-blind trial conducted in Sub-Saharan Africa early after meeting the key endpoints. This PURPOSE1 clinical trial evaluated lenacapavir as a PrEP among cisgender women. Science, the academic journal and outlet for scientific news, has named lenacapavir as 'Breakthrough of the Year' based on these study results.
- Company
- AstraZeneca Korea recertified Innovative Pharma Company
- by Whang, byung-woo Jan 07, 2025 06:05am
- AstraZeneca Korea announced today that it has successfully extended its certification as a 2024 Innovative Pharmaceutical Company by the Ministry of Health and Welfare. This marks the third consecutive recertification since the company was first certified in 2018, and recognizes the company's steady R&D investments and achievements made through global collaborations. With the extension, AstraZeneca Korea will be maintaining its status as an Innovative Pharmaceutical Company for another three years, until 2027. The Innovative Pharmaceutical Company certification system, which is organized by the Ministry of Health and Welfare, is based on the ‘Special Act on Fostering and Supporting the Pharmaceutical Industry,’ which reviews companies with high R&D investment ratios and excellent performance in developing new drugs. Certified companies can receive various support, including points for R&D support, preferential drug pricing, and tax benefits. Through its Open Innovation strategy, AstraZeneca Korea has been strengthening its collaboration with local researchers and companies to contribute to the development of the Korean pharmaceutical industry. In particular, the approval of durvalumab for the first-line treatment of biliary tract cancer in 2022 resulted from clinical trials led by local researchers and is considered a successful global collaboration model. Also, AstraZeneca Korea was recognized for its rapid response to the health crisis during the COVID-19 pandemic. The company invests around 20% of its annual revenue in clinical research, with more than 180 clinical studies underway in Korea. In addition, the company has continued to invest in R&D by conducting clinical trials on next-generation innovative drugs such as antibody-drug conjugates (ADCs), radioconjugates, and cell gene therapies in Korea. “The extension of the Innovative Pharmaceutical Company certification is an achievement of our long-standing collaboration with the Korean healthcare industry,” said Sehwan Chon, Country President of AstraZeneca Korea. ”We will continue to work closely with Korean research institutes and companies to create a patient-focused healthcare ecosystem and expand our innovative pipeline.” Chon added, “We look forward to further collaborating with the government, academia, and industry to raise the global profile of Korea's healthcare industry.”