- LOGIN
- MemberShip
- 2025-12-22 17:40:49
- Company
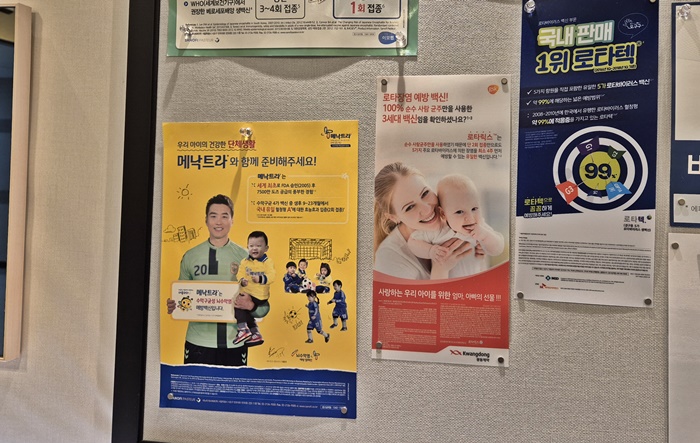
- Meningitis B vaccine Bexsero is released in Korea
- by Moon, sung-ho Jul 25, 2024 05:51am
- Competition in the 'meningococcal' vaccine market, which is mainly vaccinated in pediatric clinics, has recently been reignited. Although its domestic market is worth less than KRW 10 billion, the emergence of next-generation vaccines is expected to spark new competition among multinational pharmaceutical companies. #This is because GSK, the market leader, has launched Bexsero (meningococcal serogroup B vaccine), a next-generation vaccine. Professor Hyunmi Kang (Department of Pediatrics, St. Mary's Hospital, Seoul) explained the clinical implications of the introduction of Bexsero at an event held by GSK on the 16th. Meningococcal meningitis is a statutory Class 2 infectious disease with a fatality rate of approximately 10-14%. It affects 500,000 patients worldwide each year. The main symptoms include headache, fever, neck stiffness, vomiting, and decreased consciousness, and is often accompanied by petechiae or purpura fulminans. 11 to 19% of recovered patients may suffer from sequelae such as hearing loss, cognitive impairment, and neurological disorders, making it an important infection to prevent. In particular, as meningococcal disease is transmitted person-to-person by respiratory droplets or secretions, vaccination is recommended for those who are about to enter a group setting. For example, new recruits and college students who will be living in dormitories may want to consider meningococcal vaccination. Other recommended populations for meningococcal vaccination include travelers and residents of meningococcal endemic areas, such as Africa, and pilgrimage travelers to Mecca, Saudi Arabia. Typical serogroups of meningococci that cause invasive meningococcal infections in humans include A, B, C, W, X, and Y. The most predominant meningococcal serogroup in Korea among these is serogroup B. From 2010 to 2016, the proportion of Meningitis B cases identified in Korea was 28%, but from 2017 to 2020, the rate rose significantly to 78%. In this scene, GSK launched Bexsero, a vaccine that prevents meningococcal serogroup B, in the Korean market 2 years after its approval in 2022. Professor Kang assessed that Bexsero can play a significant role in addressing the unmet need in the field as it prevents meningococcal serogroup B. "Globally, meningococcal infections are most prevalent in infants under one year of age compared to other age groups,” explained Professor Kang. “It causes bacterial meningitis and sepsis, and one to two out of 10 survivors also experience brain damage, hearing loss, and limb loss.” "The prevalence of meningococcal serogroups varies across countries and time periods, so it is not easy to predict. In Korea, serogroup B meningococcal infection cases have increased in recent years, increasing the need for its prevention.” In Korea, GSK is leading the meningococcal vaccine market. The vaccines, which are non-reimbursed, cost KRW 150,000. The first quadrivalent meningococcal vaccine in Korea, GSK’s Menveo has been dominating the market with sales of KRW 5.2 billion based on IQVIA last year. Sanofi's Menactra is also available, but the vaccine only generated KRW 500 million in sales during the same period. In addition, Sanofi received domestic approval for Menquadfi Inj (meningococcal (A, C, Y, W) tetanus toxoid-conjugate vaccine) earlier this year. "In countries such as the United Kingdom, Portugal, and Canada, the importance of preventing disease through immunization has been emphasized due to the high prevalence of meningococcal B," said Joon Bang, Director of Medical Affairs at GSK Korea. "The predominance of meningococcal B in Korea has made it necessary for us to introduce a vaccine to prevent infections caused by meningococcal B.” "We are pleased to be able to contribute to the prevention of meningococcal disease caused by serogroup B, which accounts for a high proportion of meningococcal disease in Korea with the launch of Bexsero. Together with Menveo, the company now owns a vaccine portfolio that can protect against a wide range of serogroups."
- Company
- 'Padcev+Keytruda' combination therapy is set to land in KOR
- by Eo, Yun-Ho Jul 25, 2024 05:51am
- Product photo of Padcev.The combination therapy of 'Padcev+Keytruda,' which is expected to bring a paradigm shift to bladder cancer treatment, will soon land in South Korea. The Ministry of Food and Drug Safety (MFDS) is reviewing the expansion of indication for Astellas Korea's Padcev (enfortumab), an antibody-drug conjugate (ADC), in combination with Keytruda (pembrolizumab), a PD-1 inhibitor that is used in immunotherapy for cancer, as a first-line treatment of urothelial cancer locally advanced or metastatic urothelial carcinoma (la/mUC). The official approval is expected soon. The combination therapy of these drugs for urothelial cancer gained attention after the presentation of its Phase 3 EV-302/KEYNOTE-A39 study results at the 2023 congress of the European Society for Medical Oncology (ESMO Congress 2023), held in October last year, and received a standing ovation. Based on the clinical results, patients treated with Padcev combination had a median progression-free survival (PFS) of 12.5 months, a primary endpoint of the study, indicating a significant improvement compared to the 6.3 months in patients treated with chemotherapy for cancer. Another primary endpoint of the study was median overall survival (OS). The patients had a median OS of 31.5 months, a twofold extension compared to the placebo. Cisplantin-eligible patients treated with Padcev combination had an OS of 31.5 months compared to 18.4 months in placebo-treated group, reducing the risk of death to 47%. Cisplantin-ineligible patients had not reached the median value, whereas the placebo-treated group had an OS of 12.7 months, reducing the risk of death to 57%. In clinical settings, 'Padcev+Keytruda' combination therapy is being considered as a replacement for a first-line treatment GemCis therapy, which has been used as the standard therapy for 30 years. Meanwhile, Padcev was approved in South Korea in March 2023 as a monotherapy for patients with locally advanced or metastatic urothelial cancer who had previous experience with platinum-containing chemotherapy or PD-1 or PD-L1 inhibitors. Astellas has applied for the inclusion of this therapy in reimbursement listing, and it has passed the Cancer Disease Review Committee of the Health Insurance Review and Assessment Service (HIRA).
- Company
- Samsung Bioepis’ Soliris biosimilar is approved in the U.S.
- by Chon, Seung-Hyun Jul 24, 2024 05:51am
- View of the Samsung Bioepis building [데일리팜=천승현 기자] 삼성바이오에피스는 미국 식품의약품국(FDA)으로부터 희귀질환치료제 ‘에피스클리’의 품목허가를 획득했다고 23일 밝혔다. 에피스클리는 미국 알렉시온이 개발한 솔리리스의 바이오시밀러 제품이다. 에피스클리는 발작성 야간 혈색소뇨증, 비정형 용혈성 요독 증후군의 치료제로 FDA 승인을 받았다. 삼성바이오에피스는 2019년 7월부터 2021년 10월까지 발작성 야간 혈색소뇨증 환자들을 대상으로 임상 3상을 통해 에피스클리와 오리지널 의약품 간 비교 연구를 수행했다. 유관 학술대회 발표를 통해 임상의학적 동등성을 입증했다. 삼성바이오에피스는 지난해 7월 에피스클리를 유럽에 출시했고 독일, 이탈리아 솔리리스 바이오시밀러 시장 점유율 1위 등의 성과를 내고 있다. 국내에서는 지난 4월부터 삼성바이오에피스가 직접 에피스클리를 판매하고 있다. 삼성바이오에피스는 오리지널 의약품의 약가 대비 절반 수준으로 솔리리스 바이오시밀러를 출시했다. 삼성바이오에피스는 이번 허가로 미국 시장에서 총 8개 바이오시밀러 제품을 승인받았다. 미국에서도 자가면역질환 치료제, 항암제, 안과질환 치료제에 이어 혈액·신장질환 치료제 분야까지 치료 영역을 확대했다. 삼성바이오에피스 고한승 사장은 “미국에서도 희귀질환 치료제를 승인받아 글로벌 수준의 R&D 역량을 인정받았다”며 “에피스클리는 바이오시밀러의 사회적 가치를 극대화할 수 있는 제품으로서 세계 최대 의약품 시장인 미국에서도 그 가치를 실현하기 위해 지속 노력하겠다”고 전했다.
- Company
- Reimb applied for new HIV drug 'Vocabria+Rekambys'
- by Eo, Yun-Ho Jul 24, 2024 05:50am
- Long-acting HIV treatment 'Vocabria+Rekambys' combination therapy aims to be listed for insurance reimbursement after receiving approval in South Korea two years ago. Industry sources said that GSK Korea and Janssen Korea have applied for reimbursement for the combination therapy of Vocabria (cabotegravir) and Rekambys (rilpivirine), which each company owns. GSK will be responsible for the overall reimbursement process. In February 2022, two drugs were approved by the Ministry of Food and Drug Safety (MFDS) as a combination therapy for the treatment of adult patients with HIV-1 infection who are virologically suppressed with no history of treatment failure and with no known or suspected drug tolerance to either cabotegravir or rilpivirine. In South Korea, Vocabria +Rekambys combination therapy was approved as injection therapy with intervals of monthly or bimonthly administration. The advantage of this combination therapy is its convenience. Previously, patients had to take a tablet formulation drug once daily for conventional HIV treatments. However, with the marketing approval of these two injectables, the treatment frequency has been reduced to monthly or bimonthly as an intramuscular injection, resulting in high patient satisfaction and reduced patient burden. These two drugs were initially developed as oral formulations and later developed as injectables. As a long-acting injection therapy, these drugs cannot cure HIV injection but target white blood cells, helping to lower and maintain AIDS virus replication. The combination therapy was approved in Europe in December 2020 after a clinical trial demonstrated its efficacy and safety in a patient group treated once every 4 weeks or once every 8 weeks. The most common adverse reactions observed in a group treated with Vocabria+Rekambys combination therapy include injection site reaction, headache, fever, nausea, fatigue, general malaise, and muscle aches. Consequently, it remains to be seen whether the government agency will approve the combination therapy of these two drugs for their advantage in convenience and whether the therapy will later become listed for reimbursement.
- Company
- Will 'Zejula' be reimbursed for HRD-positive ovarian cancer?
- by Eo, Yun-Ho Jul 23, 2024 05:48am
- Product photo of Takeda Pharmaceuticals Korea Whether the insurance reimbursement criteria for 'Zejula,' a PARP inhibitor, will include 'HRD-positive' is gaining attention. Sources said that Takeda Pharmaceuticals Korea is negotiating the price with the National Health Insurance Service (NHIS) for the Poly ADP-ribose Polymerase (PARP) inhibitor, Zejula, which is used to treat ovarian cancer. The drug price negotiation is intended to expand reimbursement for the drug. Zejula is currently reimbursed for use as maintenance therapy in patients with BRCA mutation ovarian cancer who have responded to first-line treatment with platinum-based chemotherapy. The company aims to add the condition of homologous recombination repair deficiency (HRD)-positive for Zejula during the negotiations. For the treatment of ovarian cancer, Zejula was the first PARP inhibitor to demonstrate efficacy by involving HRD-positive patients in clinical studies. However, the reimbursement was limited to BRCA mutation. Since then, the company has gathered significant data on Zejula in HRD-positive patients. In a phase 3 PRIMA follow-up study, predicted variables related to progression-free (PFS) in Zejula-treated patient group were analyzed. Based on the results, predicted variables for long-term PFS after the use of Zejula for first-line maintenance therapy were found to include having a BRCA mutation or HRD, FIGO staging, the primary site of tumor, and the number of non-target lesions with conditions. Patients treated with Zejula who have BRCA mutation or are HRD-positive are highly likely to maintain PFS for over two years. Patients who are tested positive for BRCA2 gene mutation or HRD had a higher odds ratio (OR) compared to other subgroup patients. In the PRIME study result, enrolling Asians (Chinese), a significant clinical treatment effect with Zejula for patients tested positive for BRCA mutation or HRD have been confirmed. In the study, Zejula-treated patients who tested positive for HRD had an ORR of 61.3%, higher than the 29.4% ORR in the placebo group. Jae Weon Kim, Professor in the Department of Obstetrics & Gynecology at Seoul National University Hospital, said, "For ovarian cancer patients who have remaining lesions, antitumor activation by PARP inhibitors is a crucial factor in delaying the progression of the disease and prolonging PFS in patients. The findings related to long-term benefits of Zejula, including improved prognosis, are encouraging."
- Company
- Opdivo approved as 1st-line Tx for urothelial cell carcinoma
- by Hwang, Byung-woo Jul 23, 2024 05:48am
- Pic of Opdivo Ono Pharma Korea and BMS Korea announced on the 22nd that Opdivo (nivolumab) has been additionally approved by the Ministry of Food and Drug Safety as a first-line treatment for urothelial cell carcinoma (UCC). The new indication is for the first-line treatment of unresectable or metastatic urothelial cell carcinoma in combination with cisplatin and gemcitabine. Patients with unresectable or metastatic urothelial cell carcinoma who have not received prior therapy are eligible to receive the combination treatment. The approval was based on the results of the Phase III CheckMate-901 study, which compared the use of Opdivo isplatin+gemcitabine combination followed by Opdivo monotherapy with the use of cisplatin+gemcitabine combination. In the study, the Opdivo combination arm demonstrated statistically significant and clinically meaningful improvements in the primary efficacy endpoints of overall survival (OS) and progression-free survival (PFS) as assessed by a blinded independent central review committee (BICR). The safety profile of Opdivo therapy in this study was consistent with the established safety profiles of the agents in previous trials and there was no new safety information. Opdivo was first approved in August 2017 as monotherapy for the treatment of patients with locally advanced or metastatic urothelial cell carcinoma whose disease has progressed after platinum-based chemotherapy. In February 2022, the drug was additionally approved as postoperative adjuvant therapy for patients with muscle-invasive bladder cancer (MIBC) at high risk of recurrence after radical resection.
- Company
- "Trodelvy gives new hope for triple-negative breast cancer"
- by Son, Hyung-Min Jul 23, 2024 05:48am
- Triple-negative breast cancer refers to a breast cancer that is negative for estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2). It is a rare cancer that accounts for about 12-15% of all breast cancer. This cancer tends to be aggressive and has a high risk of metastasis and recurrence, leading to poor diagnosis. However, patients with this type of cancer have relied on cytotoxic anticancer medicines, the first-generation cancer treatment. They were unable to benefit from the latest cancer treatments, such as antihormone therapies and targeted cancer therapies, because all the receptors that could be targeted were negative. Trodelvy, a Trop-2 protein targeting antibody-drug conjugate (ADC), has opened a road for a new treatment for patients with metastatic triple-negative breast cancer. Trop-2 protein is a cell membrane antigen that is highly expressed in breast cancer and overexpressed in over 90% of triple-negative breast cancer. Trodelvy binds with Trop-2 protein and releases cytotoxic agents inside the cancer cells. It has the advantage of minimizing damage to healthy cells while maintaining the beneficial effects of targeted cancer therapies and cytotoxic anticancer medicines. In the multinational phase 3 clinical study, Trodelvy significantly improved overall survival (OS), progression-free survival (PFS), and objective response rate (ORR). In May, Trodelvy obtained approval from the Ministry of Food and Drug Safety (MFDS) and launched in South Korea. (From the left) Dr. Sohn, Joo Hyuk, Professor in the Department of Internal Medicine at Yonsei Cancer Hospital·Dr. Aditya Bardia, Professor in the Department of Medicine at UCLA Health Jonsson Comprehensive Cancer Center. Daily Pharm met with Dr. Aditya Bardia, the first author of 'ASCENT' clinical study and Director of Translational Research Integration and Professor in the Department of Medicine at UCLA Health Jonsson Comprehensive Cancer Center, and Dr. Sohn, Joo Hyuk, Professor in the Department of Internal Medicine at Yonsei Cancer Hospital and Korean Cancer Study Group (KCSG)'s Head of Breast Cancer Committee, to look at recent therapy trends for triple-negative breast cancer and clinical use of Trodelvy. Q. For a long time, there has been a high demand for new treatment options for triple-negative breast cancer. What is the reason for the difficulty in developing treatments? [Dr. Bardia] Triple-negative breast cancer shows the most aggressive characteristic among breast cancers, and it occurs in relatively young patients. Cytotoxic anticancer medicines are mainly used for the treatment because it is difficult to use targeted therapies due to potential therapeutic targets such as ER, PR, and HER are all negative. The problem is anticancer agents do not work efficiently in patients with metastatic cancer. Such difficulties contributed to high unmet needs for new drugs among breast cancers. [Dr. Sohn] Triple-negative breast cancer can be categorized as a diagnosis of exclusion. It refers to all breast cancer types that do not test positive for hormone receptor or HER2. Within the type, subtypes also exist. Therefore, the cancer does not exhibit consistent characteristics, posing difficulty in developing a generalized drug to be used for triple-negative breast cancer. The number of patients is relatively small, and a biologically verified target has not been identified; therefore, a treatment has not been developed. The disease itself shows aggressiveness, and patients tend to have poor diagnoses because anticancer chemotherapy that was developed decades ago is used. Q. What are the advantages Trodelvy for treating triple-negative breast cancer, where new drug development has been slow? Dr. Sohn, Joo Hyuk, Professor in the Department of Internal Medicine at Yonsei Cancer Hospital. [Dr. Bardia] Triple-negative breast cancer is negative for three receptors, ER, PR, and HER, but it does not entail that there are no receptors. Trodelvy is a treatment that targets Trop-2 protein, which is known to be overexpressed in over 90% of triple-negative breast cancer. Trodelvy can target cancer cells more efficiently than conventional standard therapies, showing superior effects. It has been designed to affect less on healthy cells, lowering toxicity and side effects that patients experience. [Dr. Sohn] Targeted therapies to date have used oncogenes that affect the progression and expansion of cancer as a target. However, Trop-2, which Trodelvy targets, is only a receptor expressed on the cell surface. Trodelvy is the first medicine to demonstrate the concept that a therapy targeting receptor expressed on cancer cell surface instead of an oncogene can be used to destroy cancer cells. In other words, it is meaningful that we have confirmed that identifying a receptor expressed on a cancer cell surface can lead to the development of a therapy. Q. According to the phase 3 ASCENT study, Trodelvy improved OS, PFS, and ORR statistically significantly compared to anticancer chemotherapies. What do these results indicate? [Dr. Bardia] Trodelvy had twofold longer OS than anticancer chemotherapy, extending patients' life expectancy. It also improved symptoms that affected patients' quality of life due to cancer, such as pain, thereby improving the quality of life during survival. The result gives patients hope to live a longer and better quality of life. [Dr. Sohn] The last drug to demonstrate the benefit of OS in triple-negative breast cancer was Halaven, released 10-20 years ago. New drugs, such as immunotherapy for cancer and PARP inhibitors, have been introduced. However, they are designed to target particular patient groups, such as PD-L1-positive patients and BRCA-mutation patients. Other than these, cytotoxic anticancer medicines are the only treatment that can be used in all patient groups with triple-negative breast cancer. Therefore, the recent data showing extended OS is historically meaningful. Patients are the only ones who can understand the differences in the number of months. Q. Has there been any change in clinical settings, including breast cancer treatment guidelines, since Trodelvy was introduced? Dr. Aditya Bardia, Professor in the Department of Medicine at UCLA Health Jonsson Comprehensive Cancer Center.[Dr. Bardia] The breast cancer guidelines of the National Comprehensive Cancer Network (NCCN) and the European Society for Medical Oncology (ESMO) foremost recommend Trodelvy as a second-line treatment for metastatic triple-negative breast cancer. In particular, Trodelvy has received a score of 5 on the ESMO-MCBS, a value-evaluation tool for anticancer medicines. Out of 37 approved treatments for metastatic breast cancer, there have been only two medicines that received a score of 5 (Trodelvy and HER+/HER2- medicine, Ribociclib). [Dr. Sohn] Previously, the effect of standard therapies for the treatment of triple-negative breast cancer was not good. When a first-line anticancer treatment had failed, the survival expectancy was only 7 months. It is a great hope to introduce a new treatment with verified survival effects to patients. Patients are welcoming treatments even if they are yet non-reimbursable. Until now, clinical settings for triple-negative breast cancer have been challenging, but this medication is likely to resolve a long-standing issue. Q. What resources are most needed to improve treatment settings for triple-negative breast cancer in South Korea? [Dr. Bardia] What we need most is to introduce the most effective new drugs regardless of the situation. We hope to enhance patients' survival duration and quality of life. I know that due to non-reimbursement, patients have limited access to Trodelvy in South Korea. I hope that National Health Insurance will be quickly applied and that access to Trodelvy in combination with other medicines will be granted. [Dr. Sohn] Patients who have private insurance or have financial well-being always choose Trodelvy. Considering the clinical data, it is a must. However, it is unfortunate that patients cannot use the medicine for economic reasons despite of the clinical evidence. I hope that healthcare financing will be allocated to those in need so that no patients are left without access to life-saving medicines. By reducing unnecessary medical spending and increasing resources for essential healthcare, South Korea can become a society that provides hope and easy access to new drugs for desperate patients. Q. What do you envision as the future approach to treating metastatic triple-negative breast cancer? [Dr. Bardia] I was once interested in AKT and PI3CA mutations and conducted two accounts of phase 3 clinical studies. However, I did not achieve fruitful outcomes. We guessed that because triple-negative breast cancer is further characterized into many subtypes, targeting AKT and PI3K3CA mutations was not effective for triple-negative breast cancer. Currently, treatments that target genetic mutations are limited to PARP inhibitors, which are offered as a first-line or second-line treatment to patients with BRCA mutations. [Dr. Sohn] Since recent studies to find new targets to treat triple-negative breast cancer are failing to demonstrate effectiveness, the remaining solution is likely to be the development of medicines targeting oncogene addiction. I heard that 350 ADCs are currently under development. New drug development is anticipated through studies about antibodies targeting cell surface receptors, cytotoxic agents, and linkers. I hope there will be more research related to combination therapies of ADCs and cytotoxic anticancer agents.
- Company
- Eisai reports degrowth for 3 consecutive years
- by Hwang, Byung-woo Jul 23, 2024 05:47am
- Eisai Korea has recorded a decline in sales of its flagship products, including its anti-cancer drug Lenvima (lenvatinib), for 3 consecutive years since 2020. The company has not seen a clear rebound since experiencing a significant drop in sales in 2022. The company’s JAK inhibitor Jyseleca (filgotinib), which was listed for reimbursement late last year, and the dementia drug Leqembi (lecanemab-irmb), which is expected to be launched by the end of the year, are gaining interest as potential drivers of the company’s performance growth. 렌비마 제품사진 Eisai’s sales last year recorded KRW139.3 billion... backsliding every year since 2021's KRW 221.9 billion In 2023, Eisai Korea’s sales in Korea totaled KRW 139.3 billion, down -0.8% from KRW 140.4 billion in 2022. This is the third consecutive year the company saw a decline since 2020. Eisai’s sales peaked at KRW 221.9 billion in 2020 before declining to KRW 212.9 billion in 2021. The company's revenue then fell to KRW 140.4 billion in 2022, a 34% year-on-year decline. During the same period, operating profit was KRW 23.2 billion in 2020, KRW 22.8 billion in 2021, and KRW 5.1 billion in 2022. However, operating profit rebounded to KRW 9.3 billion last year, largely due to a decrease in the cost of goods sold (KRW 77 billion to KRW 73.3 billion) and selling, general and administrative expenses (KRW 58.2 billion to KRW 56.6 billion). The decline in growth is attributed to the company’s decline in sales of Lenvima, which is used to treat liver and thyroid cancer, along with a decline in sales of its existing product portfolio. According to IQVIA, Lenvima’s sales have declined from KRW 15.8 billion in 2021 to KRW 13.6 billion in 2022, then to KRW 10.3 billion in 2023. In addition, the fact that Lenvima is facing patent challenges from generic companies is also discouraging news for Eisai in the long term. Currently, Boryung is challenging Lenvima’s patents from multiple directions. Eisai is raising its barriers by registering new patents, but Boryung is also actively responding, reaffirming its determination to launch its generic early. In addition, sales of Pariet, a GERD drug, were KRW 14.6 billion last year, down slightly from the KRW 15.1 billion the previous year. Equfina’s sales grow after reimbursement...Aricept’s sales exceeded KRW 70 billion for the third consecutive year Although Eisai’s sales declined for the third consecutive year, there is room for its rebound. Its Aricept, its key product, showed solid sales, and Equfina’s sales growth and the introduction of new drugs are expected to also work in favor of the company. First, sales of its Parkinson's disease treatment Equfina (safinamide mesilate) have grown every year since its reimbursement in February 2021. Equfina, which generated KRW 800 million in sales in its first year of coverage, has grown at an average annual rate of about KRW 2 billion, reaching KRW 4.8 billion in sales last year. It is also positive that Aricept (donepezil hydrochloride), a dementia treatment, has shown solid sales for 3 consecutive years since posting sales of KRW 70.4 billion in 2021. ArIcept sold KRW 73.8 billion last year, up 1% from KRW 72.9 billion in 2022 A particularly promising part of Eisai’s dementia portfolio is its dementia drug Leqembi, which is expected to launch by the end of the year. Leqembi, which was approved by the MFDS in May, is said to have utilized the ‘approval-reimbursement linkage system’ for the drug’s reimbursement. The system allows for a drug to apply for reimbursement approval to the Health Insurance based on the results of the MFDS’s safety and efficacy review before approval. This reduces the insurance drug price review period and enables faster market entry. In addition, Jyseleca, which entered the reimbursement system in November last year and passed the drug committee (DC) of major hospitals including tertiary hospitals, is also a promising item. Jyseleca was initially approved for rheumatoid arthritis and moderate-to-severe active ulcerative disease, and while several JAK inhibitors are competing with the same indications, Jyseleca is priced competitively at less than 90% of the weighted average price, which is expected to drive sales growth.
- Company
- Atopic dermatitis drugs get expanded indication for infants
- by Eo, Yun-Ho Jul 23, 2024 05:47am
- Dupixent and Adtralza. New atopic dermatitis drugs are currently being considered for expanded use in infants and young children. First, Sanofi Korea's 'Dupixent (dupilumab)' will be reimbursed for treating infants aged 6 months beginning next month. The company has recently concluded the drug price negotiation, and on July 19th, Dupixent was incorporated into the Ministry of Health and Welfare (MOHW)'s revised regulations on the criteria and scope of National Health Insurance. Dupixent's expanded reimbursement for young children was in high demand. Previously, the Severe Atopic Dermatitis Association (SADA) issued a statement urging the coverage of Dupixent for young children aged 6 months to younger than 6 years with severe atopic dermatitis. 85-90% of atopic dermatitis manifests symptoms at the age of five, and for severe cases, the disease persists until adulthood and relapses. However, treatments approved for children under the age of five are limited to topical treatments, and the patients with symptoms uncontrolled with topical treatments have limited treatment options due to long-term skin retractions and infection risks. Leo Pharma Korea is preparing to secure an indication for its 'Adtralza (tralokinumab),' which became reimbursement-listed in May, to treat young children. On July 1st, Leo Pharma was approved for phase 3 clinical trials to evaluate the safety and effectiveness of Adtralza in combination with a topical corticosteroid in patients with moderate-to-severe atopic dermatitis aged 2-12 years and 6 months to younger than 2 years. Adtralza can be reimbursed when prescribed for treating adult patients (18 years or older) and adolescent patients (12-17 years) with chronic severe atopic dermatitis whose symptoms persisted for over three years. Meanwhile, the phase 3 ECZTRA3 and ECZTEND studies demonstrated the efficacy and safety of Adtralza. The ECZTRA3 study compared Adtralza to placebo in patients aged 18 years and older with moderate-to-severe atopic dermatitis who had an inadequate response to previous topical therapy or require systemic therapy. Dupixent's efficacy in young children was demonstrated in the LIBERTY AD PRESCHOOL Phase 3 trial. The results confirmed that Dupixent significantly improved skin pathology. At 16 weeks, 28% of patients treated with Dupixent in combination with topical corticosteroids (TCS) showed a score of 0 or 1 point in the Investigator's Global Assessment PN-Stage (IGA PN-S), demonstrating a significant improvement in atopic dermatitis compared to 4% of the placebo group. Consequently, it met the primary efficacy endpoint.
- Company
- Hyperlipidemia Drug Leqvio’s nears market entry in KOR
- by Hwang, Byung-woo Jul 23, 2024 05:47am
- Novartis’s Leqvio’s (Inclisiran), is preparing to enter Korea’s market as the first siRNA therapy, armed with its convenience of twice a year administration. However, in a situation where there are already many treatments for hyperlipidemia available on the market, the high cost of Leqvio compared to existing treatments may act as a hurdle, regardless of its advantages. Pic of Leqvio Leqvio is a first-in-class siRNA therapy that was recently approved in Korea as an adjunctive therapy to diet in patients with primary hypercholesterolemia (heterozygous familial and non-familial) or mixed dyslipidemia. It utilizes a naturally occurring siRNA to reduce LDL-C in the blood by inhibiting the production of PCSK9 protein, which raises LDL-cholesterol. It is injected directly by a healthcare provider twice a year, reducing the fear and discomfort of self-injection. In the three Phase 3 studies that confirmed the effectiveness of Leqvio - ORION-9, ORION-10, and ORION-11 -Leqvio reduced the LDL-C level by 47.9%, 52.3%, and 49.9% compared to placebo at Day 510, respectively. In all 3 studies, the safety profiles of Leqvio and placebo did not show statistically significant differences. In ORION-18, which was conducted on Asian patients including 24% Korean patients, Leqvio achieved a 57.17% LDL-C reduction compared to placebo at Day 330. These results have been driving Leqvio’s rapidly growing global sales. Leqvio’s global sales in the first half of the year amounted to $333 million, prompting Novartis to raise its full-year profit forecast. The company is expected to target the market armed with its twice-a-year dosing advantage in Korea. The question is how it can compete with the other competitors that are already being reimbursed. Higher cost compared to competitors...receiving reimbursement crucial for market suceess For Novartis, its first and utmost priority will be to receive reimbursement. According to industry sources, Novartis is considering a list price of KRW 1.5 million for a single dose of Leqvio. If so, the cost of the twice-a-year treatment is expected to be in the range of KRW 2 to 3 million. Considering how it is administered 3 months after the initial dose, and then every 6 months thereafter, the drug can cost even more in the first year. Current direct competition is Amgen's Repatha (evolocumab), which has overlapping indications for hypercholesterolemia and mixed dyslipidemia. Repatha’s sales had been around KRW 4.2 billion in 2021, KRW 7 billion in 2022, and KRW 10.5 billion in 2023, according to IQVIA. Repatha is priced at KRW 121,000 per dose with reimbursement. The recommended dose is 420 mg once every two weeks or once a month (three doses). Therefore, it costs 1.42 million won based on the higher dose of 420 mg once a month. The price gap becomes even wider when compared to Viatris’ Lipitor, which has expanded its indication and is recorded as a top-selling drug in Korea every year. Lipitor is priced at KRW 640 per 10mg tablet, which means it costs KRW 233,600 when taken once a day. Based on the largest dose of 80 mg, which costs KRW 1,523 per tablet, it still costs 558,895 won a year. In the end, the therapeutic effect of Leqvio and the convenience it provides to patients who have difficulty managing their medications will be the key to its future market competitiveness. "I think Leqvio will be in demand among elderly patients who have difficulty taking drugs consistently and those with poor prognosis. However, most patients are seeing significant therapeutic effects with existing medications and exercise," said a cardiology professor from A Hospiatl in Gyeonggi-do. In some cases, patients who are well-controlled on Repatha can maintain their levels well with once-a-month Repatha injections. From a personal point of view, the cost versus convenience of dosing is a difficult decision."