- LOGIN
- MemberShip
- 2025-12-18 03:16:03
- Policy
- ALS drug Qalsody is approved in Korea with a condition
- by Lee, Hye-Kyung Aug 22, 2025 06:07am
- The ALS treatment ‘Qalsody (tofersen)’ has been approved under the condition that the results of its therapeutic confirmatory clinical trial be submitted later. According to the advisory council’s review results regarding the safety and efficacy of Qalsody, which was released by the Ministry of Food and Drug Safety on the 20th, the council saw consensus on the need to grant conditional approval for Qalsody, given how ALS worsens over time and treatment options are limited. Biogen's Qalsody is a nucleic acid therapy that binds to SOD1 mRNA in patients with ALS caused by mutations in the superoxide dismutase 1 (SOD1) gene, reducing the synthesis of mutated proteins (SOD1). It received domestic approval from the MFDS on the 20th of this month. According to the CPAC meeting results, experts noted that ALS is a highly severe disease that can be fatal without treatment, and that there are no specific medications available for the condition at the present. In particular, Qalsody’s indication is limited to ALS patients with SOD1 gene mutations. While the mechanism of action involves binding to mRNA, entering the nucleus, and inhibiting SOD1 expression, there were opinions that it is difficult to directly evaluate or reflect the actual SOD1 secreted externally. A member of the CPAC stated, “Based on the submitted data, the drug seems to show an effect when NfL correction is applied. In neurodegenerative diseases, biomarkers can sufficiently explain the extent of neural damage, and as there is scientific evidence on their effect, conditional approval was deemed appropriate.” Another member explained, “This disease is a rare and severe condition with no available treatments in the country, and existing approved drugs are primarily used for symptom relief. Given the clinical trial results based on the NfL biomarker and its potential to control the disease, we deemed that the benefits are significant and agree to grant a conditional approval.” However, there was also an opinion that the completion date of the conditional Phase III clinical trial should be considered, as patients with SOD1 mutations account for less than 3% of all ALS patients, which may require a longer patient recruitment period. Experts also suggested that conditional approval is necessary to provide treatment opportunities for domestic patients, as the drug is already in use overseas. In other words, the council saw that the safety and efficacy of the drug are deemed acceptable based on the data submitted by the pharmaceutical company, and conditional approval is needed to allow patients to benefit from the treatment as soon as possible. Meanwhile, Qalsody was approved in Korea through the accelerated approval process, the Global Innovative products Fast-Track (GIFT), as the 31st product.
- Policy
- MFDS's bill on stable supply of essential drugs in review
- by Lee, Jeong-Hwan Aug 20, 2025 06:22am
- A bill to add “medicines that are essential for healthcare and require stable supply” and “medicines with similar therapeutic effects with no alternative treatments” to the list of national essential medicines, thereby resolving the issue of unstable supply of medicines, is likely to pass the Health and Welfare Committee's legislative subcommittee. At the subcommittee meeting held on the morning of the 19th, the subcommittee members and the Ministry of Food and Drug Safety agreed on the intent of the legislation, but there were some disagreements over the specific wording that should be used to codify the definition, so the subcommittee agreed to pass the bill after going through the amendment process on the same day. The subcommittee members and the MFDS also agreed to accept a provision to revise the designation method for essential medicines to be designated by the Minister of Health and Welfare and the Minister of Food and Drug Safety after consultation with the National Essential Medicine Stable Supply Council. The bill also includes provisions to include “linking drug distribution information” in the scope of the Comprehensive Drug Management Center's duties and to allow the MFDS director to request the Drug Management Information Center to provide and link drug distribution information. On the morning of the same day, the subcommittee members decided to merge the bills proposed by Representative Sun-min Kim of the People Power Party and Representative Mi-hwa Seo of the Democratic Party of Korea and continue deliberations. However, as further discussions on the bill are scheduled at the afternoon subcommittee meeting, there is a possibility that it could pass the subcommittee on the same day if an agreement is reached between the government and the subcommittee members. The bill expands and revises the definition and scope of essential medicines and establishes a legal basis for managing distribution information to contribute to the stable supply of essential medicines. Expanding the definition of essential medicines to strengthen management of drugs with unstable supply The current law defines essential medicine as “medicines that are essential for health and medical care, such as disease control and radiation disaster prevention, but whose stable supply is difficult to ensure through market functions alone, and which are designated by the Minister of Health and Welfare and the Minister of Food and Drug Safety in consultation with the heads of relevant central administrative agencies.” Rep. Sun-min Kim's bill proposed revising the definition of essential medicines to “drugs that are essential for maintaining the national health system, such as disease control and radiation disaster prevention, or that are essential for health and medical care and require a stable supply, as designated by the Minister of Health and Welfare and the Minister of Food and Drug Safety in consultation with the National Essential Medicine Stable Supply Council.” Representative Mi-hwa Seo's bill proposed amending the definition to “medicines that are essential for health and medical care, such as disease control and radiation disaster prevention, but whose stable supply is difficult to ensure through market functions alone, or drugs for which there are no substitutes with similar therapeutic effects, as designated by the Minister of Health and Welfare and the Minister of Food and Drug Safety after consultation with the National Essential Medicine Stable Supply Council pursuant to Article 83-4, Paragraph 3.” The MFDS agreed to reflect both Kim and Seo’s bills and submitted a proposed amendment to the relevant clause. The MFDS proposed to revise the bill so that essential medicines would be designated by the Minister of Health and Welfare and the Minister of Food and Drug Safety after consultation with the National Essential Medicine Stable Supply Council, and to define essential medicine as drugs that are essential for maintaining the national health system, drugs that are essential for health care but difficult to supply stably through market forces alone, and drugs for which there are no substitutes with similar therapeutic effects. The members of the subcommittee raised the need to define essential medicines in one line rather than listing them individually as proposed in the MFDS amendment, and requested a further amendment. The subcommittee is expected to resume its review of the bill in the afternoon based on the amendment. Distribution information linkage included in the scope of the Integrated Pharmaceutical Management Information Center’s duties The MFDS agreed to add “distribution information linkage” to the scope of the Integrated Pharmaceutical Management Information Center’s duties and to allow the MFDS Minister to request the provision and linkage of distribution information in consultation with the director of the information center. The MFDS also accepted provisions to add “drugs that are not designated as essential medicines but require stable supply due to temporary increases in demand” to the scope of drugs managed by the National Essential Medicine Stable Supply Council and to add monitoring of essential drug supply and demand trends to the duties held by the Minister of Health and Welfare and the Minister of Food and Drug Safety. The MFDS also expressed its opinion regarding the provision to specify the composition of the National Essential Medicine Stable Supply Council in the law. Under the current law, the council is composed of 20 government members, including one chairperson, with the remaining details to be specified in the implementing regulations. Rep. Sun-min Kim’s proposal stipulates that the council shall consist of 30 members, including two chairpersons, with government and private-sector members, and that private-sector members shall constitute a majority. Rep. Mi-hwa Seo's proposal stipulates that the council shall consist of 30 members, including one chairperson, with government and private-sector members. The MFDS proposed a council composition similar to Rep Kim’s proposal, consisting of 30 members, including two chairpersons, but added patient group representatives as recommended by Rep Seo. The subcommittee plans to resume deliberations in the afternoon, as it believes that there has not been sufficient discussion on the details of the bill.
- Policy
- MOHW proposes an alternative to law on generic substitution
- by Lee, Jeong-Hwan Aug 19, 2025 06:11am
- A revision to the Pharmaceutical Affairs Act that would allow pharmacies to report generic substitution to the Health Insurance Review and Assessment Service (HIRA) through its work portal is likely to pass the National Assembly. The background to the sudden increase in the likelihood of legislation is that the Ministry of Health and Welfare submitted its own alternative proposal to the National Assembly regarding the bill to simplify generic substitution by pharmacies and changed its position to conditional approval (acceptance) on the premise that its alternative proposal would be adopted. If the National Assembly accepts the alternative proposal submitted by the MOHW, the simplification of post-notification of generic substitution will be legislated in the Pharmaceutical Affairs Act, a law, rather than as an Enforcement Rule, a subordinate law. The alternative submitted by the MOHW stipulates that the Minister of Health and Welfare shall be able to support related administrative tasks, such as post-notification of generic substitution, and that such support tasks may be entrusted to the Health Insurance Review and Assessment Service. Rather than specifying the method of post-notification of generic substitution in the law, the proposal broadly stipulates that the MOHW shall provide support and legalize the framework for entrusting the MOHW's duties to HIRA. On the other hand, HIRA maintained its cautious stance, citing concerns for patient safety in the event of an accident involving a medication misadventure and the lack of legal grounds for entrusting the task to HIRA. This follows the Ministry of Health and Welfare’s submission, on the 18th, of its opinion on the amendment to the Pharmaceutical Affairs Act (aimed at simplifying generic substitution) to the National Assembly Health and Welfare Committee’s First Legislative Subcommittee. The law to simplify generic substitution was proposed by Representative Young-seok Seo of the Democratic Party of Korea and Representatives Sujin Lee and Byung-deok Min of the same party. The Health and Welfare Committee plans to hold the 1st Subcommittee meeting on the 19th to review the bill. The main contents are a provision to change the term “substitute dispensing” to “generic name substitutions” and a provision to expand the scope of post-notification of substitute prescriptions to HIRA. The change in terminology provision has been strongly opposed by the medical community, including the MOHW, and it is unlikely to pass the National Assembly. The provision to simplify generic substitution by expanding the scope of post-notification was once rejected by the subcommittee after the MOHW expressed its need for cautious review. However, the MOHW submitted a legal alternative it had drafted itself to the subcommittee and changed its position to support the legislation on the condition that it be passed by the National Assembly as is. The simplification of post-notification of generic substitution is expected to take effect on February 2 next year, as MOHW has already confirmed the revision of the Enforcement Rules of the Pharmaceutical Affairs Act, and the possibility of the National Assembly revising the Pharmaceutical Affairs Act has also increased. The MOHW has once again expressed its cautious stance on legislation that would require HIRA to notify prescribing doctors of the results of post-notification of generic substitution by pharmacies. The MOHW argued that this is not in line with the purpose and scope of HIRA's establishment and that the increase in the notification period could raise concerns about the safety of drug use. The MOHW also pointed out that the amendment to the Enforcement Rules of the Pharmaceutical Affairs Act allows post-notification via HIRA's information system in addition to telephone and fax. However, in consideration of the need to clarify the legal basis for the HIRA information system currently being developed by the MOHW and the necessity of substitute dispensing in response to drug supply uncertainties, the MOHW stated that an alternative plan would be necessary to establish a basis for HIRA's policy support. So the alternative submitted by the MOHW to the National Assembly stipulates the establishment of “support for generic substitution under Article 27-2 of the Pharmaceutical Affairs Act” and, in Paragraph 1, stipulates that the Minister of Health and Welfare may provide support for matters specified by MOHW ordinances, such as support for post-notification of generic substitutions. Paragraph 2 allows the Minister of Health and Welfare to entrust HIRA with the task of providing support for post-notification of generic substitution, and paragraph 3 stipulates that the details and methods of support and other necessary matters shall be determined by MOHW ordinances.. However, HIRA maintained its cautious stance on the bill. The logic behind its need for cautious review is that if post-notification generic substitution is carried out through HIRA, the notification period will increase, and if an accident occurs due to a lack of awareness on the part of doctors, this will raise concerns about patient safety. In addition, HIRA argued that it can only perform tasks entrusted to it by other laws and regulations in accordance with Article 63 of the National Health Insurance Act, and therefore, a separate basis for entrusting tasks related to generic substitution notifications is necessary. Furthermore, it also argued that unique identification numbers in accordance with the Personal Information Protection Act, regulations on the handling of sensitive information, and provisions exempting HIRA from liability for medication misadventure are necessary. d The Korean Pharmaceutical Association in favor, Korean Medical Association and Korean Hospital Association oppose The Korean Pharmaceutical Association supported the bill. On the other hand, the Korean Medical Association and the Korean Hospital Association maintained their opposition. The Korean Pharmaceutical Association predicted that allowing HIRA to notify doctors and dentists electronically would eliminate administrative inconveniences and streamline procedures, thereby promoting generic dispensing, considering the difficulty of notifying doctors and dentists when pharmacists substitute drugs due to factors such as failure to include fax numbers or failed phone connections. The Korean Medical Association argued that pharmacists could arbitrarily change medications without the consent of doctors, which could undermine the right of doctors to prescribe medications, make it difficult to respond quickly to adverse drug reactions, and raise questions about the accountability of the dispensed generic substitutions and their side effects. The Korean Hospital Association also opposed the bill, arguing that notifying just the HIRA of generic substitutions would make it difficult for doctors and pharmacists to share information about generic substitutions, which could delay the necessary treatment for patients in cases of inappropriate generic substitutions.
- Policy
- Periodic drug price system reform included as national task
- by Lee, Jeong-Hwan Aug 18, 2025 06:02am
- President Lee Jae-myung attended the National Planning Committee The government has selected a policy to improve the drug price calculation system and establish a periodic drug price adjustment mechanism as part of its national policy task, with the goal of ensuring the sustainability of health insurance, and is pushing ahead with its implementation. Depending on the specific details of the national policy task to be established in the future, it is noteworthy that this could lead to additional post-marketing management regulations, such as a price reduction mechanism for generic drugs with expired patents, which is a highly concentrated area in the domestic pharmaceutical industry. To build a primary care-based health and care system, the government plans to gradually expand the local primary care physician model starting next year (2026) and adopt the institutionalization of telemedicine and public electronic prescription transmission systems as national policy tasks through social consensus. According to the National Assembly and the medical community on the 13th, the National Planning Committee has adopted such policy directions as national policy tasks. Transition to a sustainable healthcare system The National Planning Committee proposed improving the drug price calculation system and establishing a periodic drug price adjustment mechanism as a means of stabilizing the sustainability of the national health insurance budget, in order to curb expenditure factors that worsen the healthcare system, such as budget leakage. The government has been managing national health insurance drug expenses by adjusting the insurance ceiling price (drug price) of new and generic drugs through the post-marketing drug management system. In particular, following research conducted last year by Professor Dong-sook Kim’s research team at Kongju National University under the Yoon administration, the Ministry of Health and Welfare recently commissioned and launched additional research on the generic drug price system following the election of President Jae-myung Lee and the appointment of MOHW Minister Eun-kyung Jeong. The ministry has entered into a direct contract with a research team led by Professor Seon-mi Jang of the College of Pharmacy at Gachon University to conduct a study titled “Reform of the Drug Price Model (Focusing on Generic Drugs).” The results of this study is expected to serve as a basis for the government's drug price reductions. The Ministry of Health and Welfare under the Lee administration also agrees that it is necessary to establish financial leeway for national health insurance by adjusting the prices of old drugs with uncertain efficacy, so there is great social interest in whether new drug price reduction mechanisms, such as the overseas reference pricing reevaluation measures will emerge. However, there are also opinions that it is difficult to judge whether generic drug prices in South Korea are high or low compared to other developed countries. The Korean pharmaceutical industry is dissatisfied that the government is focused solely on establishing policies to reduce drug prices and is relatively neglecting policies that award premiums on drug prices. Ultimately, the pharmaceutical industry is expected to respond depending on how the details and direction of the national policy agenda are decided. Expansion of telemedicine and establishment of a public electronic prescription system The National Planning Committee has also selected the promotion of public health through primary care-based health management as a national policy task. The goal is to extend the healthy life expectancy of citizens by improving the management rate of chronic diseases through measures such as the expansion of local primary care physicians, the expansion of telemedicine, and the establishment of a public electronic prescription transmission system. The community-based local primary care physician model is planned to be expanded in phases starting in 2026, with the core elements being the provision of comprehensive health management based on multidisciplinary teams and innovative compensation based on performance. The Democratic Party of Korea has submitted a bill to the National Assembly to strengthen primary care and institutionalize the primary care physician system, titled the “Special Act on Strengthening Primary Care” (“Primary Care Special Act”, proposed by Representative In-soon Nam), ahead of the implementation of the Integrated Care Act. The Integrated Care Act and the Primary Care Special Act are expected to serve as the legal and administrative basis for building a society that provides national health care based on primary care. In particular, the National Planning Committee will institutionalize telemedicine based on social consensus and establish a system of telemedicine and remote consultation at public health centers targeting medically underserved areas in rural and fishing villages. Four bills to formally institutionalize telemedicine pilot projects (by Reps. Bo-yoon Choi, Jae-joon Woo, Jin-sook Jeon, and Chil-seung Kwon) are pending in the National Assembly, and the Health and Welfare Committee is expected to review them in the near future. The first subcommittee review is expected to take place as early as the 19th. The National Planning Committee is also expected to include a plan to establish and operate a public electronic prescription transmission system in its national policy task from 2027, based on opinions gathered from the medical community and the Pharmaceutical Association, in line with the institutionalization of telemedicine. The institutionalization of telemedicine and the introduction of public electronic prescriptions were also part of President Jae-myung Lee 's presidential campaign promise. Meanwhile, the National Planning Committee's national policy task must undergo final review by the relevant government ministries and the State Council before it can be finalized.
- Policy
- Gilead’s Yescarta approved in KOR...3rd CAR-T therapy
- by Lee, Hye-Kyung Aug 14, 2025 06:13am
- The third CAR-T therapy has been approved in Korea. The Ministry of Food and Drug Safety approved Gilead Sciences Korea's Yescarta (axicabtagene ciloleucel) today (13th). Yescarta is a CAR-T therapy that received approval from the U.S. FDA in 2017 and the European EMA in 2018. Last year, the EMA approved it as a second-line treatment for patients with adult diffuse large B-cell lymphoma and B-cell acute lymphoblastic leukemia. In June, the FDA expanded the indication for Yescarta to include patients with follicular lymphoma. In Korea, after the drug was designated as an orphan drug by the MFDS in September last year, it has been undergoing the formal approval process. According to a brief issued by the Korea Biotechnology Organization, Yescarta is currently the CAR-T therapy with the highest market share worldwide. Posting sales of USD 1.5 billion (approximately KRW 2 trillion) last year, Yescarta ranked first with a 40% share of the entire CAR-T market. It was followed by Novartis' Kymriah posting USD 500 million (approximately KRW 700 billion), Johnson & Johnson's ‘Carvykti’ at USD 500 million, BMS's ‘Abecma’ at USD 470 million (approximately KRW 650 billion), and Gilead Sciences' ‘Tecartus’ at USD 370 million (approximately KRW 500 billion). Kymriah and Carvykti have already been granted marketing authorization in Korea. Meanwhile, according to an analysis presented at the American Society of Clinical Oncology (ASCO) 2023 Annual Meeting, at a median follow-up of 47.2 months, the overall survival (OS) in the Yescarta treatment group had not yet reached the median, while the placebo group had a median OS of 31.1 months, indicating a statistically significant 27% lower risk of death with Yescarta. The estimated 48-month overall survival rate was 54.6% for Yescarta and 46.0% for the control group, with Yescarta demonstrating consistent survival benefits across pre-specified subgroups, including age, primary resistance, early relapse, and high-grade B-cell lymphoma.
- Policy
- New drug approval fees ₩410mil in KOR
- by Lee, Hye-Kyung Aug 13, 2025 06:07am
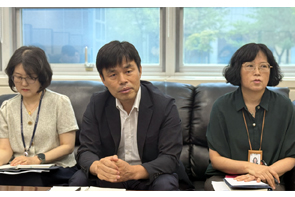
- Since the new drug approval fee was significantly increased to KRW 410 million starting this year, a total of 14 new products containing 10 ingredients have been submitted for approval. Although the specific product names cannot be disclosed, dedicated teams have been formed for 6 chemical drug substances and four biopharmaceutical substances, and the review process is currently underway. On the 12th, Young-joo Kim, Director of the Drug Approval Division at the Ministry of Food and Drug Safety, So-hee Kim, Director of the Director of the Cardiovascular Drug Division of the Drug Review Department, and Jae-ok Kim, Director of the Biological Products Division of the Bio and Herbal Medicine Review Department, met with specialized media journalists to provide an interim briefing on the new drug approval and review innovation process that began this year. , Young-joo Kim, Director of the Drug Approval Division at the Ministry of Food and Drug Safety, So-hee Kim, Director of the Director of the Cardiovascular Drug Division of the Drug Review Department, and Jae-ok Kim, Director of the Biological Products Division of the Bio and Herbal Medicine Review Department On January 1, the MFDS raised the new drug approval fee to KRW 41 million, formed dedicated teams for each item, expanded face-to-face consultations and reviews between companies and approval reviewers for items submitted for approval to a maximum of 10 times, and shortened the manufacturing and quality control evaluation and actual condition survey of new drug manufacturing facilities (to within 90 days). The increased approval fees were to be used mostly to hire high competency reviewers, and the MFDS has established a policy to operate a professional, swift, transparent, and predictable approval review system so that the process from new drug approval application to license issuance can be completed within 295 days. The new drug approval and review process begins with a pre-submission consultation, followed by the submission of a product license application. A dedicated team of approximately 15 members is then formed for each product. Actual meetings begin within 2 weeks of the submission of the application. GMP inspections for new drugs are also completed within 90 days of the submission date. On January 31, multinational pharmaceutical company Eli Lilly applied for marketing authorization for its new breast cancer drug “Inluriyo Tab (imlunestrant),” and a total of 10 substances are currently under review. While actual marketing authorizations are not completed in the order of application submission, for Inluriyo, if the innovative approval scheme for new drugs is applied, approval could be granted as early as November or by December at the latest. Director Young-Joo Kim stated, “While I cannot comment on the approval process for specific products, we are striving to complete the approval process within 295 days from the date of submission of the marketing authorization application in accordance with the new drug approval and review procedures. Despite the increase in new drug approval fees, we anticipate that the number of marketing authorization applications submitted will be similar to previous years.” As of August, applications for new drug approvals for 10 ingredients have been submitted, and based on the usual number of applications, applications for 20 ingredients were submitted in 2023 and 19 ingredients in 2024. The MFDS believes that if this trend continues, the number of item approval applications will remain similar to those of previous years. Kim added, “Until last year, when requests for supplementary data were made, everything was handled via documents. However, now, there are over 10 face-to-face meetings from preliminary consultations to supplementary data submission requests, and all of this process is documented.” However, despite the significant increase in fees, only 15 to 17 dedicated staff members are being assigned to expedite approvals. This is why, when a meeting is held regarding supplementary materials, everyone has to gather for a meeting lasting over an hour and a half. Director Jae-ok Kim explained, “One hour and a half may seem short, but when supplementary materials are submitted, pharmaceutical companies also select the points they want to focus on and ask questions. The meeting lasts about an hour and a half, with the purpose of the supplementary data request being explained and any questions being answered.” In the case of new drug approval fees, most of the increased amount will be used to cover the pay of high competency reviewers. Currently, there are 31 high competency reviewers hired specifically for the new drug team, which is close to the total quota of 36. The new drug dedicated team is composed of a team leader who is the head of the approval department, a product manager from the approval department, and specialists in safety and efficacy, quality control, GMP (good manufacturing practice), and GCP (good clinical practice), rendering the need to reinforce the specialized review staff. Director Young-joo Kim said, “With the increase in new drug approval fees, the cost of review is borne by the beneficiaries. The MFDS has a total of 370 reviewers, including those for medical devices, and about 10% of them are high competency reviewers.” However, as high competency reviewers are hired as public employees rather than civil servants, it is difficult for them to provide stable service. As a result, they may only receive training on high competency review techniques and move to other organizations within a few years. Director Jae-ok Kim added, “The current review staff is going through a transitional period. High competency reviewers cannot be immediately deployed; they must first undergo training, work as assistant reviewers, and then transition to head reviewers." He also pointed out that “this process is causing an overload of work for existing review staff.” Director So Hee Kim also emphasized, “Since the system is still in its initial stages, mid-level managers are facing significant challenges. While hiring high-skilled reviewers is important, expanding the pool of personnel capable of fulfilling mid-level management roles is also necessary.” In this regard, Director Young-joo Kim said, “It is important to enable high competency reviewers hired as public officials to be appointed civil servants,” adding, “We plan to consult with other ministries and request that the number of civil servants be continuously increased.” Although the MFDS is applying the new drug approval fee hike only to new drugs, it plans to gradually expand it to other items. President Jae-myung Lee's remarks also support this stance. At a recent cabinet meeting, the president stated, “Insufficient review costs and a shortage of personnel are causing delays in new drug approvals, which is a loss for society as a whole. Increasing review costs is a way to expand the budget without increasing the financial burden.” Director Young Joo Kim said, “The MFDS understands that the intention is not to further raise the new drug approval fees, but to expand the fees to items other than new drugs to increase revenue. We are in ongoing discussions with government ministries and related industries on items for which fees can be raised based on principles such as the novelty and complexity of the substance.”
- Policy
- Smokers at 54.5 times higher risk of SCLC than non-smokers
- by Lee, Tak-Sun Aug 12, 2025 06:13am
- A study has found that 30-year smokers have a 54.5 times higher risk of developing small cell lung cancer than non-smokers. The National Health Insurance Service (NHIS) Health Insurance Policy Research Institute announced on the 11th the results of a comparative analysis of cancer incidence risk and attributable risk by cancer type among individuals with the same level of polygenic risk score (PRS) and similar living environments, focusing on major cancers with high incidence rates in Korea. The study found that the risk of developing small cell lung cancer among current smokers (30 years or more, 20 pack-years or more) was 54.5 times higher than that of non-smokers, significantly higher than colorectal cancer (1.5 times), liver cancer (2.3 times), and stomach cancer (2.4 times higher). T Cancer risk according to smoking history (hazard ratio) This study was jointly conducted by the Health Insurance Policy Research Institute (Director Seongin Jeong) and Yonsei University Graduate School of Public Health (Professor Seon-ha Ji's research team). The study analyzed data from 136,965 participants who underwent health screenings at 18 private screening centers nationwide from 2004 to 2013, linking health screening results, polygenic risk scores (PRS), central cancer registry data, and health insurance eligibility data, and followed the participants until 2020. The analysis of cancer incidence risk showed that even when general characteristics, living environments, and PRS were at the same level, the incidence risk of smoking-related cancers (small cell lung cancer, squamous cell lung cancer, and squamous cell laryngeal cancer) was higher in the smoker group than that of other cancers. Compared to non-smokers, current smokers with a smoking history of “30 years or more and 20 pack-years or more” had a significantly higher cancer incidence risk: 54.5 times higher for small cell lung cancer, 21.4 times higher for squamous cell lung cancer, and 8.3 times higher for squamous cell laryngeal cancer. However, the risks were 2.4 times higher for stomach cancer, 2.3 times higher for liver cancer, and 1.5 times higher for colorectal cancer. The extent to which smoking contributes to the development of small cell lung cancer was found to be 98.2%, followed by 88.0% for squamous cell laryngeal cancer, and 86.2% for squamous cell lung cancer, confirming that smoking is the primary cause of the cancers targeted in the tobacco litigation. In contrast, the extent to which smoking contributes to the development of colorectal cancer is 28.6%, stomach cancer 50.8%, and liver cancer 57.2%, indicating that smoking contributes significantly less to these types of cancer compared to the cancers subject to litigation, and that other factors play a major role. Genetic factors contribute only 0.4% to the development of squamous cell lung cancer, whereas they account for 7.3% of colorectal cancer and 5.1% of stomach cancer, indicating that genetic factors have a significantly greater influence on these cancers compared to squamous cell lung cancer, with respective differences of 18.3 times and 12.8 times. Sunmi Lee, Director of the Health Insurance Policy Research Division at the Health Insurance Policy Research Institute, emphasized, “The results of this study show that smoking contributes significantly more to the development of lung cancer and laryngeal cancer compared to other types of cancer, while genetic factors play an extremely minor role. This further clarifies the causal relationship between smoking and the development of lung cancer and laryngeal cancer.”
- Policy
- Will RSV vaccines be included in the NIP?
- by Whang, byung-woo Aug 08, 2025 06:03am
- With the RSV (respiratory syncytial virus) vaccine being released in Korea this year, interest in its inclusion in the National Immunization Program (NIP) has been gaining attention. According to the National Assembly's legislative information system, on the 6th, Rep. Yong-ki Jeon of the Democratic Party of Korea introduced a bill titled “Partial Revision of the Infectious Disease Control and Prevention Act,” which contained provisions on including RSV in the NIP. Rep. Jeon explained, “The current law stipulates diseases subject to mandatory vaccination for the prevention of infectious diseases with high prevalence rates and frequent outbreaks. For influenza, a representative disease subject to mandatory vaccination, the prevalence rate of respiratory viruses from 2015 to 2019 was 11.7% to 21.5%.” He went on to point out that “Even though the prevalence rate of respiratory syncytial virus (RSV) and acute respiratory infections caused by RSV during the same period was 11.7% to 20.1%, indicating a risk level similar to that of influenza, mandatory vaccinations are not currently being administered for RSV.” Accordingly, the legislative intent of the bill is to contribute to improving public health through infectious disease prevention by stipulating that mandatory vaccinations be administered for acute respiratory infections as well. If the bill is passed, it is expected to accelerate the inclusion of RSV vaccines into the National Immunization Program (NIP). Currently, Sanofi's Beyfortus, an RSV preventive antibody for infants and young children, and GSK's Arexvy, an RSV vaccine for adults aged 60 and older, have been approved and released in South Korea. Currently, the KDCA maintains that the inclusion of RSV vaccines in the NIP requires sufficient discussion and review. During last year's government audit, Rep. Myeong-ok Seo (People Power Party) of the National Assembly Health and Welfare Committee questioned the KDCA about the necessity of including RSV vaccines in the NIP, and the KDCA responded that it would “conduct a thorough review in the mid- to long-term through expert and vaccination committee deliberations.” In particular, the NA’s inquiry referred to Beyfortus, the only preventive antibody approved for RSV at the time. Still, the KDCA also mentioned that Beyfortus is not classified as a vaccine. The KDCA explained, “The NIP includes vaccines, so to introduce new formulations such as preventive antibodies into the program, there must be social consensus on the NIP itself.” RSV preventive antibodies work by injecting passive antibodies into the human body to trigger an immune response. Although the goal and mechanism are similar to those of vaccines, strictly speaking, they are not traditional vaccines. Under these circumstances, it appears that the KDCA is taking a cautious approach to determining whether a drug of a different class can be incorporated into such existing programs. In this case, if the bill is passed, it is likely that Arexvy, which has been approved as a vaccine, will be approved. According to the medical community, the Korean Society of Infectious Diseases is reportedly discussing guidelines for adult RSV vaccination. However, if the proposed amendment is passed, discussions will likely take place within the broader framework of contributing to the promotion of public health through the prevention of infectious diseases. With the support of the legislation, it could also have a positive impact on securing the budget necessary for NIP discussions. However, the proposed amendment includes provisions regarding the submission of a cost estimation report, which may require the submission of economic evaluation data for the vaccine in the future.
- Policy
- Gov’t sets criteria for drug shortage prevention
- by Lee, Hye-Kyung Aug 07, 2025 06:06am
- Prime Minister Min-seok Kim chaired the 7th Biohealth Innovation Committee at the Government Complex Seoul on the 5th The government will improve the criteria to raise the prices of drugs essential for patient treatment. Specifically, it will establish detailed evaluation criteria for price adjustment requests submitted by pharmaceutical companies that deem the current insurance price ceiling unreasonable. Prime Minister Min-seok Kim chaired the 7th Biohealth Innovation Committee at the Government Complex Seoul on the 5th and discussed measures to foster Korea into a biohealth powerhouse with government and private sector members. The meeting covered major issues such as improving drug price standards, revising the cost calculation method for exit prevention drugs, and expanding support for late-stage clinical bio venture funds. First, the criteria for designating drugs subject to drug shortage prevention measures will be revised upward to align with the changing pharmaceutical market environment in consideration of how their stable supply would affect the population as well as the fiscal expenditures required from the national health insurance. There have been calls from the field that the current criteria for designating drugs subject to drug shortage prevention measures, which have been in place since 2017, lack practicality, and there is a consensus that the minimum threshold amount needs to be revised to reflect factors such as inflation rates. In response, the government plans to publicly disclose by the end of the year a price adjustment criteria for such essential medicines, which will comprehensively consider factors such as the medical necessity, availability of alternatives, the number of suppliers of the same formulation (including whether the product is de facto the only drug supplied), and the supply situation of the drug, when evaluating price increases for drugs whose maximum prices have been announced and deemed significantly unreasonable by pharmaceutical companies. The government stated that through this, it expects to realistically adjust the minimum benchmark amount for selecting drugs to prevent withdrawal from the market by reflecting factors such as inflation rates, and to evaluate whether to adjust the maximum price based on drug price adjustment criteria that comprehensively consider actual supply conditions, thereby improving the profitability of essential drugs for patient care. Additionally, based on results of a recent study on improving the system for drug shortage prevention drugs, the government will revise part of the Standards for the Determination and Adjustment of Drug Prices (Appendix 5) to improve the cost calculation method for such medications, with the revised standards to be implemented in the first half of next year. The system improvements that will be made through revisions to the relevant regulations are expected to ensure preservation of appropriate production costs for drug shortage prevention drugs, leading to an increase in drug prices and enhanced supply stability for such drugs. Discussions on support for biotech companies were also held. The government is considering the establishment of a specialized fund for companies with ongoing or complete Phase III clinical trials that possess candidate substances or pipeline for innovative new drugs and biobetters. This is expected to enable domestic pharmaceutical and venture companies with excellent capabilities to secure sustained investment for Phase 3 clinical trials, which require significant time and costs, thereby increasing the likelihood of developing blockbuster new drugs. The government also plans to establish a basic-specialized-advanced step-by-step support system to help domestic companies enter the global market in response to the rapidly changing global pharmaceutical environment and provide customized consulting services. In addition, the government plans to provide specialized information through workshops on approval and licensing of advanced pharmaceutical and biotech products, produce online educational videos, and publish expert articles. Discussions were also held on expanding customized cost support in response to regulatory tightening in advanced countries such as the United States and the EU. To prepare for the tight regulations in advanced countries such as the FDA and MDR, the government plans to adjust the schedule for announcing customized cost support programs (from March 2024 to January 2025) to extend the support period for selected companies in the same year. Also, the government plans to change the project operation method to allow continuous cost support without additional project solicitations after monitoring the first-year performance when selecting this year's support recipients. Through these measures, domestic companies will be able to alleviate the financial burden and human resource shortages associated with certifications for the U.S. FDA and European MDR. In order to respond to the rapidly changing global pharmaceutical environment, the government plans to establish a step-by-step (basic-specialized-advanced) support system for domestic companies to advance into the global market and provide customized consulting services. Discussions were also held on a project being carried out by the Korea Disease Control and Prevention Agency (KDCA). The KDCA’s project supports the development of mRNA vaccines for pandemic preparedness in order to secure a vaccine platform that can be developed at a rapid pace in preparation for future pandemics. This project is a large-scale research project with a total budget of KRW 505.2 billion, which will support research and development tasks from preclinical to Phase III clinical trials over four years (2025-2028) with the goal of obtaining approval for a COVID-19 mRNA vaccine by 2028. The preliminary feasibility study was exempted in 2024, and the total budget and project period were finalized in March this year through a review of the appropriateness of the project plan. The KDCA confirmed the selection of four non-clinical trial project institutions in April and is currently supporting research and development to enter Phase I clinical trial in December of this year. To ensure the smooth implementation of the project, the KDCA's mRNA Vaccine Development Support Team and the Korea Health Industry Development Institute are planning the project and managing the performance targets. If the COVID-19 mRNA vaccine is developed through the project, it will not only ensure a stable supply of vaccines for high-risk groups but also enable the rapid development of vaccines within 100 to 200 days using Korea’s own mRNA vaccine technology in the event of a future pandemic.
- Policy
- H1 Pharma exports amounted to $5.38B
- by Lee, Hye-Kyung Aug 07, 2025 06:05am
- In the first half of this year, healthcare industry exports increased by 13.2% compared to the same period last year, reaching $13.79 billion, an all-time high for a half-year period. By sector, exports were led by cosmetics at $5.51 billion (+14.9%), pharmaceuticals at $5.38 billion (+20.5%), and medical devices at $2.91 billion (△0.6%). The Korea Health Industry Development Institute (KHIDI, President: Soon-do Cha) announced these export figures for pharmaceuticals, medical devices, and cosmetics for the first half of 2025 on August 6. Exports of pharmaceuticals increased by 20.5% year-over-year to $5.38 billion, driven by a surge in biopharmaceutical and vaccine exports. Biopharmaceutical exports (accounting for approximately 63.4% of total pharmaceutical exports) recorded $3.41 billion, a 27.4% increase year-over-year. Notably, exports saw a significant increase to the United States ($980 million, +41.4%), Hungary ($520 million, +26.8%), Germany ($470 million, +66.7%), Switzerland ($460 million, +76.9%), and the Netherlands ($250 million, +719.8%). H1 2025 Healthcare Industry Exports (unit: $1 million, %) Vaccine exports ($170 million, +53.3%) grew significantly in Sudan ($20 million, +397.3%), South Sudan (from $0 in H1 2024 to $10 million in H1 2025), and Congo (from $0 in H1 2024 to $10 million in H1 2025). According to Lee Byung-kwan, head of KHIDI's Biohealth Innovation Planning Division, "In the first half of 2025, healthcare industry exports were driven by all-time high half-year performances in the cosmetics and pharmaceutical sectors," and added, "In the second half, export growth is also expected to continue, driven by the expanding global demand for key products like biopharmaceuticals and basic cosmetics." Lee emphasized, "As external uncertainties such as changes in the U.S. tariff policy persist, it is crucial to monitor market trends and respond with caution and strategy carefully."